- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
The Life-Saving Surgery That Saved The Twin Brothers

Credits: King's College Hospital NHS Foundation Trust
Eight-month-old twins from Hayward Heath, West Sussex, recently met the surgeon who saved their lives even before they were born. The BBC reports how their mother, Katerina Ahouansou, at six months pregnant, during a routine scan, uncovered a serious issue with their development and blood supply.
Doctors diagnosed the twins with twin-to-twin transfusion syndrome or TTTS. It is a condition where one twin received more blood and nourishment than the other due to uneven blood vessel distribution in the placenta. In case there is no medical intervention, it could be fatal for both the twins.
A Specialist Steps In
This is when Ahouansou was referred to Professor Kypros Nicolaides at King’s College Hospital in London. Professor Nicolaides is a pioneer in fetal medicine and he specializes in a laser procedure that redistributes blood supply between twins in cases of TTTS.
When Ahouansou was scanned, Nicolaides observed that one of the twins were significantly smaller than the other. "There was a very high chance that if we did not intervene, both twins could die," he recalled.
An Operation No Less Than A Miracle
The life-saving laser surgery was performed and within a week the doctors saw an improvement with the twin who was smaller in size. When the twins were born, they weighed 1.5kg and 1.7kg. To recognize the efforts by the surgeon, Ahouansou named them Kai Kypros and Asher Nicolas after Professor Kypros Nicolaides.
Ahouansou also expressed deep gratitude for the professor's expertise and called him "proof that miracles can be performed by people who are devotees to their profession."
Professor Kypros Nicolaides has been at King’s College Hospital since 1980 and is widely regarded as a leader in fetal medicine. His groundbreaking research and development of screening and surgical techniques have saved countless lives.
Through his dedication, Professor Nicolaides has given many families hope, demonstrating how medical advancements continue to improve survival rates for complex fetal conditions like TTTS.
More about Twin-to-twin Transfusion Syndrome
As per the John Hopkins Medicine, TTTS is a rare pregnancy condition that affects identical twins or other multiples. It happens in pregnancies where twins share one placenta and a network of blood vessels that supply oxygen and nutrients essential for development in the womb. These pregnancies are known as monochorionic.
Sometimes, the blood vessels in the placenta are unevenly distributed, causing an imbalance in blood flow between the twins. The donor twin loses more blood than it receives, leading to malnutrition and potential organ failure. Meanwhile, the recipient twin gets an excess of blood, putting strain on the heart and increasing the risk of cardiac complications.
Impact on the Donor Twin
The donor twin loses blood volume (hypovolemia), reducing kidney function and urine production. This leads to low amniotic fluid levels (oligohydramnios) or, in severe cases, a complete absence (anhydramnios). Without proper blood circulation, the donor twin faces cardiovascular issues, increasing the risk of death.
Impact on the Recipient Twin
The recipient twin experiences excess blood volume (hypervolemia), causing increased urination and excessive amniotic fluid (polyhydramnios). The overworked heart struggles to handle the surplus blood, leading to cardiovascular dysfunction, heart failure, and, in extreme cases, death.
Danica McKellar Said She Loved How Her Placenta Tasted; Why Do Some People Eat It?

Credits: Wikimedia Commons
Danica McKellar, American actress said she was embarrassed to admit that she liked tasting her placenta. While she did not go into childbirth thinking she was going to taste her placenta, she says she is glad she did so.
She said this while explaining her surprising postpartum culinary experience in a conversation with Bobby Bones on The BobbyCast.
"My doula said, do you want to taste the placenta? I'd just given birth. And I'm like, sure. I mean, you're not even, you're not in your right mind. She gave me a piece of it. Bobby, it was like the best filet mignon that I have ever tasted. But more," she said.
She continued that she was embarrassed about how much she loved it. "It was bizarre. I thought, what is this, some sort of weird satanic...Am I a cannibal?"
She is now mom to 15-year-old son Draco Verta, who she shares with her ex-husband and composer Mike Verta.
Why Do People Eat Placenta?
A 2014 BBC report notes that placenta sustains life in the womb and leaves the mother once it has served its purposes after the childbirth. The nutrients that have passed from mother to fetus over the months of pregnancy are still packed inside the placenta and should not be wasted. Instead, the raw placenta, many believe, could provide what the mother needs to recover from childbirth and begins breastfeeding.
Some women, as the BBC report notes, are also choosing to drink the placenta in a fruit smoothie within hours of giving birth. While others keep it cool and send it off to be dried and made into capsules, or ripping chunk of it and placing it by their gums.
As per Mayo Clinic, some people believe that eating placenta can help them recover from postpartum depression. However, the US Centers for Disease Control and Prevention issued a warning against taking placenta capsules. The warning was based on the case in which newborn developed an infection called group B streptococcus after the mother took placenta capsules.
The mother was thought to be infected with group B strep bacteria that came from the placenta because the capsules tested positive for the bacteria. Then the infection spread to the infant. Group B strep can cause serious illness in newborns. That may include a severe infection called sepsis. Group B strep also can lead to meningitis. Meningitis is an infection that affects the lining of the brain and spinal cord.
This infection happens when one processes their placenta and it could expose the placenta to bacteria or viruses.
Placenta And What It Holds
The placenta contain several hormones, including oxytocin, estrogen, progesterone, and relaxin. It is also rich in protein, amino acids, and minerals. However, the claims of people saying that it is healthy and should be consumed after delivering a child to avoid postpartum depression have not been fully tested. There are however cases where animals other than humans eat placenta after birth as it could reduce there labor pain. However, the same has not been proven in humans.
Leucovorin Prescriptions Surge After White House Mentions It For Autism Use, Parents Struggle To Find Drug
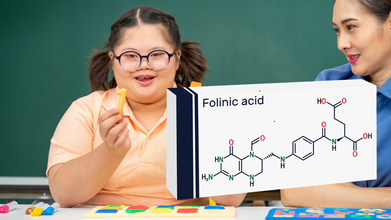
Credits: Canva and iStock
Leucovorin, a high-dose vitamin - folinic acid, were mostly used for treating toxic side effects of chemotherapy, until last year when the White House touted it as a potential treatment for some children with autism. New prescriptions for leucovorin double within weeks of announcement and parents have been trying hard to get it prescribed. This is also because many doctors have been hesitant to prescribe a chemotherapy medicine for childhood autism. They have also stated that not enough evidence is available to prescribe this drug officially.
CNN reported that in Austin, Texas, Meagan Johnson spent four days calling pharmacies across the region searching for leucovorin for her three-year-old son Jack, who has autism. She contacted nearly 40 pharmacies around her home in Pflugerville, hoping to locate the medication.
The effort came after a neurologist agreed to prescribe leucovorin on a trial basis. Johnson’s hope was simple: even a small improvement in her son’s communication would mean a lot. At age three, most children can say hundreds of words, but Jack speaks only about 20, many of which only his mother understands.
However, getting the prescription turned out to be far harder than obtaining it.
Across the United States, pharmacies have been reporting growing difficulty keeping leucovorin tablets in stock. Online support groups for parents of autistic children are now filled with posts from families searching for the medication or asking where it might still be available.
Although leucovorin is not approved specifically for autism, some small studies have suggested that it may help certain children who have unusually low levels of folate in the brain. Families who have tried it report possible improvements in language and social interaction.
A study published in The Lancet found that prescriptions for leucovorin doubled within weeks of the public remarks and remained elevated through early December. Researchers analysed electronic medical records covering nearly 300 million patients to identify the trend.
Experts say such spikes can quickly strain the supply of inexpensive generic drugs.
A Classic Demand-Driven Shortage
Pharmacy supply specialists describe the leucovorin situation as a demand-side shortage. Unlike manufacturing disruptions, these shortages happen when demand rises faster than manufacturers can increase production.
Generic drug manufacturers typically plan production schedules a year or more in advance. Because leucovorin had historically been a niche medication, companies were not prepared for a sudden surge in prescriptions.
As demand increased, pharmacies began running out of tablets. Many manufacturers have placed the drug on allocation or backorder, meaning pharmacies can only order limited quantities.
To ease the pressure, the US Food and Drug Administration allowed temporary imports of leucovorin tablets from Canada and Spain. However, the drug has not yet been officially listed on the FDA’s national drug shortage database, a designation that could trigger additional measures to boost supply.
Families Searching For A Treatment
For parents like Johnson, the debate over research evidence matters less than the possibility of progress.
After days of phone calls, a CVS pharmacist finally located a supply at another branch nearly an hour away. Johnson drove the distance to pick up the medication and gave Jack his first dose that same evening.
The moment brought relief, but also frustration.
Drug shortage advocates say the situation was predictable. Because leucovorin is inexpensive and historically prone to shortages, any sudden increase in demand could easily disrupt supply.
Still, families continue to search for it.
The Working Mother’s Double Shift: Office Deadlines, Baby Duties and Endless Guilt | Women’s Day Special

Credit: Canva
Imagine standing at the starting line of a race, dressed properly with the best running shoes and ready to give your best. Yet, as the race begins, you notice that while half of the runners beside you have a clear path ahead, yours is filled with obstacles -- a dirty diaper, a crying baby, piles of laundry, a sink full of dishes, an empty fridge, cooking to be done, and countless other responsibilities.
If you pictured that correctly, you have just imagined the race of a man (with a clear road) and a woman’s race — more precisely, the race of a mother.
In 2019, the chairman of the Mahindra Group, Anand Mahindra, famously posted on the social media platform X, featuring the race of a working man and a woman, sparking a conversation on gender equality.
On International Women’s Day, women are given flowers, cake, or chocolates as a matter of appreciation for their seemingly multi-talented roles, but hardly does that go into consideration by families, partners, and workplaces.
Sanjana (name changed), a marketing professional from Bengaluru, was overjoyed as she held her first baby after a bout of four years of trying, several treatments, and constant pressure from family and society.
Speaking to HealthandMe, she said that the joy, however, was short-lived when she decided to get back to work.
“I had to figure out the support system -- what will I do, what will my husband do, and from what time to what time I need to keep a nanny. When I joined, I realized there was zero flexibility. I couldn’t leave work before completing a nine-hour shift and had to travel two hours back and forth. I was exhausted by the time I got back home, but nothing was ever ready for me to relax. It felt like the beginning of another shift after getting home.
"The baby would be eagerly awaiting me, and my mother's guilt was at its peak, so even though I was physically exhausted, I would still want to give him my time. Since I could never pick my baby up or get him or his meals ready for daycare, I felt guilty asking my husband to do more,” she told HealthandMe.
Shopping for groceries, refilling the baby’s necessities, making sure food is cooked as per everyone’s taste, and ensuring the baby’s routine isn’t disturbed are major responsibilities of most mothers.
“For a new-age mother, every day is a battle between love and responsibility. She meets deadlines with sleepless eyes and hugs her child with a tired heart. Judged at work, questioned at home -- yet she shows up. Not perfect, not rested, but relentless,” said Shivangi (name changed), an IT professional from Delhi.
While a woman’s quiet strength is often marked as victory, facing warzone-like situations every day -- from boardrooms to bedtime stories, meeting deadlines and doctor visits, balancing ambition, and affection -- takes a heavy toll on her mental and physical health.
HealthandMe spoke to Mimansa Singh Tanwar, Clinical Psychologist and Head of the Fortis School Mental Health Program at Fortis Healthcare, on the struggles of new mothers.
“New mothers often find themselves stretched thin while balancing the constant nurturing needs of the child and trying to realign their life with a change in their self-identity. This is a period of huge transition, both emotionally and physically, where new mothers tend to experience feelings of guilt for not being able to do enough for the child or not doing it the ‘right’ way. They often find themselves divided between work and the child’s needs once they resume work. It’s important to be gentle with yourself and accept that you don’t have to do everything perfectly,” Tanwar said.
“Being a mother is itself a moment of pure joy, but for many new mothers, it is also the beginning of a relentless balancing act. There are significant underlying hormonal and neurochemical changes that affect mood and behavior. Sleepless nights, multiple feeding schedules, household expectations, multitasking, and trying to match the ‘ideal perfect mother’ image can have a significant impact on the mind.
"Mothers often put their own needs quietly at the bottom of the list, which affects their overall well-being,” Dr. Sameer Malhotra, Principal Director - Department of Mental Health and Behavioral Sciences, Max Super Specialty Hospital, Saket, told HealthandMe.
Is There a Motherhood Penalty?
Several studies have pointed out how returning to the workplace as a new mother can be a vulnerable time for women. Many are likely to face baby blues, characterized by feeling weepy or anxious. Maternal labor force participation also sees a dip after motherhood.
A 2021 study published in the Journal of Development Economics showed that motherhood caused a sharp decline in employment in Chile, with 38 percent of working women leaving the workforce and 37 percent still out a decade later.
Global estimates by UN Women and the International Labor Organization (ILO) showed that more than 2 million mothers left the labor force in 2020.
During the pandemic, about 113 million women aged 25–54 with partners and small children were out of the workforce in 2020. This figure is astonishing, particularly when compared to their male peers (13 million of whom were out of the workforce, up from 8 million before COVID-19).
A 2007 study published in the American Journal of Sociology found that mothers face penalties in hiring, starting salaries, and perceived competence, while fathers can benefit from being a parent. Mothers were six times less likely than childless women and 3.35 times less likely than childless men to be recommended for hire. Mothers were also recommended a 7.9 percent lower starting salary than non-mothers.
How Mothers Can Help Themselves
Tanwar urged women to “be gentle with yourself and accept that you don’t have to do everything perfectly.”
Other measures include:
- Setting small, realistic goals
- Resting whenever possible
- Asking for help
- Sharing responsibilities with family members
- Staying connected with supportive family or friends
- Talking openly about your feelings to ease the load
“Simple self-care, even a few quiet moments each day, helps restore calm and energy. It is important to remember that looking after yourself is a key part of caring well for your baby,” Tanwar said.
© 2024 Bennett, Coleman & Company Limited

