You Have Heard Of Blood Thinning, But Do You Know Blood Thickening Can Also Make You Sick?
Recently, a friend's relative was admitted to the hospital after experiencing recurring discomfort and unstable blood sugar levels. Initially, it appeared to be a routine diabetes complication, but it turned out she had something unexpected—her blood was thickening to such an extent that it was making her sick.While blood thinning is often discussed in the context of diabetes and cardiovascular conditions, the dangers of blood thickening, or hypercoagulability, remain largely overlooked.
This woman in her late 60s living with diabetes, was in danger of suffering a life-threatening complications from abnormally clotting blood. Her story highlights an often overlooked medical issue: thick blood can prevent proper circulation, increase the risk of thrombosis, and contribute to all sorts of health complications, including some that prove fatal if ignored.
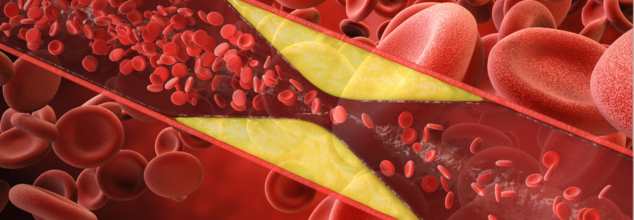
Blood must be in a fine balance to be able to circulate properly and clot when needed. But when there is an imbalance of blood proteins and cells, it becomes too thick. This is called hypercoagulability, and it makes the blood more prone to clotting, which can clog the blood vessels and cause serious health issues like strokes, heart attacks, and deep vein thrombosis.
While blood is homogeneous in appearance, it contains a mix of different components, such as red and white blood cells, platelets, proteins, and clotting factors. When these components exist in a greater quantity than normal, the blood becomes thicker, thus harder for the heart to pump it effectively through the body.
What Causes Blood to Thicken?
There are a number of reasons why blood may become thick, and although some are inherited, others are acquired later in life. Some of the most important causes include:
Overproduction of Blood Cells: Too many red blood cells (polycythemia vera) or platelets can cause thick blood.
Underlying Illnesses: Diseases such as cancer, lupus, and diabetes can interfere with blood clotting mechanisms.
Too Much Clotting Protein: Some people overproduce clotting proteins, which puts them at risk of thrombosis.
Smoking: Smoking harms blood vessels and lowers the body's capacity to form anticoagulant factors.
Inflammation: Elevated inflammatory markers, frequently found in chronic conditions such as diabetes, contribute to clot formation.
Because there is no one definition of "thick blood," physicians diagnose it according to the underlying condition causing abnormal clotting.
Link Between Diabetes and Thick Blood
Diabetes patients are especially vulnerable to thickening of the blood because of elevated glucose, lipid, and inflammatory cytokine levels in the blood. Diabetes encourages the development of plaque in arteries, thus enhancing the likelihood of lethal clots. The condition, which is referred to as thrombosis, may clog arteries and veins and result in fatal complications.
When an individual has diabetes, their platelets (small blood cells responsible for clotting) become hyperactive, and the risk of clot formation becomes higher. Poor circulation and long-term inflammation are also contributing factors. Scarily, research indicates that almost 80% of individuals with diabetes will eventually perish from clot-related complications.
Symptoms of Thick Blood
Most individuals are unaware of their thick blood until a blood clot develops. In others, a family history of clotting disorders will lead to testing before symptoms arise. Warning signs can include:
- Blurred vision
- Dizziness
- Frequent headaches
- Easy bruising
- High blood pressure
- Shortness of breath
- Fatigue and lack of energy
- Excessive menstrual bleeding (in women)
- Itching skin
- Gout (a type of arthritis brought on by an excess of uric acid in the blood)
If you have unexplained clotting, multiple pregnancy loss (greater than three first-trimester miscarriages), or a family history of clotting diseases, see a physician for screening.
What Tests Can Detect Hypercoagulability?
In diagnosing thick blood, physicians review the complete medical history and perform blood tests in phases. Some of the most frequently performed tests are:
Complete Blood Count (CBC): Tests for elevated red blood cell or platelet counts.
Activated Protein C Resistance Test: Finds the presence of Factor V Leiden, which is a genetic mutation linked with blood clotting disorders.
Prothrombin G20210A Mutation Test: Finds abnormality in the blood clotting factors.
Antithrombin, Protein C, and Protein S Levels: Assists in finding conditions like lupus anticoagulants.
These tests being expensive and highly specific, physicians would typically start with more general screening tests and proceed to more specialist diagnostics.
How Can You Reduce the Risk of Thick Blood?
Although some reasons for thick blood are genetic and cannot be avoided, life-style changes and medical treatment may decrease risks in people with diabetes or other predisposing factors. Preventive strategies include:
- Circulation is improved and blood kept from becoming sluggish through exercise.
- Thickening of the blood can result from dehydration, so proper hydration with water is crucial.
- Keeping glucose and lipid levels in check can minimize risks of clot formation.
- Smoking harms blood vessels and facilitates clot formation.
- Eating foods with omega-3 fatty acids (fish, flaxseeds, and walnuts) helps in minimizing inflammation and enhancing circulation.
- In certain individuals, physicians might recommend blood thinners such as aspirin or anticoagulants.
Ignoring to symptoms of thick blood may result in more dangerous complications. It is critical to detect them early with routine check-ups and blood work, especially for patients with diabetes, cardiovascular disease, or a family history of blood clotting diseases.
If you suspect that you have thick blood or have clotting-related symptoms, see your doctor right away. Early detection and treatment will avert fatal disorders like stroke, heart attack, and deep vein thrombosis.
© 2024 Bennett, Coleman & Company Limited

