Credits: Wikimedia Commons
Why Psoriasis Causes Inflammation? This Is What You Can Do
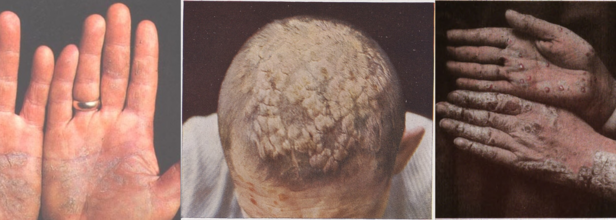
Psoriasis is a chronic immune-mediated inflammatory disease, meaning inflammation plays a key role in its development. While its exact cause remains unknown, psoriasis affects up to 3% of adults in the United States. It primarily leads to skin symptoms such as raised plaques and discoloration but can also impact other areas, including the joints and eyes.
What Causes Inflammation in Psoriasis?
In individuals with psoriasis, the immune system malfunctions, causing inflammatory cells to accumulate in the dermis, the middle layer of the skin. This dysfunction also speeds up skin cell production in the outer layer (epidermis).
Normally, skin cells take about a month to grow and shed, but in psoriasis, this process occurs in just a few days. Instead of shedding, the excess skin cells build up, resulting in symptoms such as plaques, scaling, redness or discoloration, and swelling.
However, psoriasis is not just a skin condition. The inflammation it causes can affect the entire body, increasing the risk of other health issues like heart disease, cancer, inflammatory bowel disease, and psoriatic arthritis.
Can Inflammation Be Treated?
Since inflammation in psoriasis is linked to immune system dysfunction, treatments aim to reduce this inflammation. Research suggests that lifestyle and dietary changes can help minimize symptoms and improve overall well-being.
Many people with psoriasis can maintain remission—periods without symptoms—by adopting these changes. In addition, medical treatments such as topical corticosteroids, injectable biologics, and oral medications work to control inflammation. The severity of psoriasis varies from person to person, so treatment needs differ accordingly.
Managing Inflammation in Psoriasis
While there is no cure for psoriasis, the following lifestyle habits may help reduce inflammation and improve symptom control.
Eating a Nutritious Diet
Diet is closely linked to inflammation. Certain dietary patterns can worsen psoriasis, while others can alleviate symptoms.
Avoid inflammatory foods: Processed foods, sugary drinks, and excessive salt or unhealthy fats may trigger psoriasis symptoms.
Follow an anti-inflammatory diet: Research suggests that a Mediterranean-style diet rich in fruits, vegetables, whole grains, and healthy fats can reduce psoriasis severity.
Maintaining a Healthy Weight
Obesity is a risk factor for psoriasis, and excess weight can worsen symptoms. Studies indicate that weight loss can reduce inflammatory markers and improve psoriasis severity. For instance, a 2020 study found that losing 12% of body weight over 10 weeks led to a 50–75% reduction in psoriasis symptoms.
Adopting Healthy Lifestyle Habits
Several habits can help lower inflammation and manage psoriasis symptoms:
Quit smoking: Smoking worsens inflammatory diseases, including psoriasis.
Limit alcohol intake: Excessive drinking contributes to inflammation and symptom severity.
Stay active: Regular movement helps reduce psoriasis severity. Sedentary lifestyles are linked to worse symptoms.
Get enough sleep: Poor sleep increases inflammation. Experts recommend 7–9 hours of sleep per night for optimal health.
Manage stress: Stress is a common psoriasis trigger. Practices like meditation and yoga can help reduce stress levels and inflammation.
When to Seek Medical Help?
If you experience a psoriasis flare-up and want to manage inflammation, consulting a healthcare provider, particularly a dermatologist, is essential. They can recommend appropriate treatments, dietary adjustments, and lifestyle changes to help reduce symptoms. Additionally, they may suggest vitamins or supplements that could support your overall health.
While psoriasis is a lifelong condition, proactive management can lead to improved quality of life and extended periods of remission.

Credits: Canva
Ignored, Misdiagnosed And At Risk: Why Women Need To Listen To Their Heart?
Even after decades of health education campaigns and medical breakthroughs, there is still one myth that dangerously persistent—the heart disease is a "man's disease." This misconception has contributed to a fatal blind spot in diagnosing, treating, and managing women across the globe. The reality is even more sinister: cardiovascular disease (CVD) is the world's biggest killer of women, killing more people annually than all cancers together.
What's even more troubling is that the problem continues to exist in the face of decades of data, research, and advocacy by groups such as the American Heart Association (AHA), who continue to raise the alarm. Women are being misdiagnosed, underdiagnosed, and undertreated—particularly young women and women of color—resulting in avoidable deaths and long-term health repercussions.
Young Women Are Facing More of Heart Disease
Once thought to be at risk only after menopause, young women are increasingly having heart attacks and other cardiovascular events. Increasingly, studies now indicate that heart disease is increasing among young women between the ages of 18 to 55, a trend that has puzzled experts and rendered emergency rooms unprepared to recognize early warning signs among this group.
These women aren't only falling ill to the disease—they're also more prone to be sicker and to fare worse than age-matched men. They face this with further delayed diagnoses, with research indicating that women wait an average of more than two days before describing heart attack symptoms, compared with 15 hours for men.
Some of the challenge is the way heart attacks manifest in women. Men usually see the hallmark symptom of crushing chest pain, but women tend to present with more insidious, unusual symptoms, such as:
- Shortness of breath
- Jaw, back, or neck pain
- Nausea or vomiting
- Indigestion
- A feeling of dread
- Unusual fatigue or palpitations
These symptoms are commonly misinterpreted—by both physicians and patients—into stress, anxiety, or gastrointestinal distress, resulting in delays in treatment. Indeed, women are less likely to be immediately provided an electrocardiogram (EKG) in the ER and frequently are released from the ER without proper diagnostics or treatment.
Why Women Are Misdiagnosed?
Apart from symptoms, the body physiology of a woman's heart is not the same as a man's, making things even more complicated. Women have smaller vessels, are more prone to microvascular disease, and have special types of heart attacks like spontaneous coronary artery dissection (SCAD) and myocardial infarction with nonobstructive coronary arteries (MINOCA). These are the kinds that don't register on standard tests, so women's heart attacks might be completely overlooked.
More disturbing is the inherent gender bias in healthcare. Studies indicate women and minorities spend more time in the ER waiting for treatment, are less likely to be hospitalized, and do not get prescribed life-saving medications following a heart attack. The AHA says 26% of women die within one year of experiencing their first heart attack, as opposed to 19% of men.
Pioneering cardiologists are dubbing it a global health crisis. A groundbreaking consensus statement by 33 specialists from the British Cardiovascular Society has provided a vision plan for closing these disparities. The statement is urging:
- Champions and specialist centers for women's heart health
- Equal diagnostics and treatments
- More women in clinical trials
- Care models that are culturally and gender-sensitive
It also draws attention to the fact that more than 3.6 million women in the UK alone suffer from ischemic heart disease, with most getting delayed or suboptimal treatment. This is replicated all over the world—from the US to South Asia—due to old-fashioned medical beliefs, societal prejudices, and ignorance.
What Women Can Do Right Now?
For far too long, women's voices—particularly when they are reporting pain or discomfort—have been ignored or trivialized. But your body remembers when something's amiss, and listening to your heart may save your life.
Here's what you can do:
Learn your risk factors—blood pressure, cholesterol, diabetes, and family history.
Speak up for yourself—question your doctor, ask for proper tests, and don't be afraid to seek a second opinion.
Pay attention to the signs—even if they don't fit the norm.
Live a heart-healthy life—eat healthfully, stay active, cope with stress, and have regular check-ups.
Women such as Stewart, a heart attack survivor and advocate for the AHA's Go Red for Women initiative, remind us that awareness alone is not sufficient. Education, action, and advocacy are needed to turn back the deadly tide of overlooked and undiagnosed heart disease in women.
Heart disease does not discriminate, yet the medical system still does. From delay in ER treatment to exclusion from clinical trials, women are perpetually an afterthought in the world of cardiovascular medicine. That has to end. Whether you are a 20-year-old woman, a mother managing stress, or a retired grandmother, your heart matters. And so does it deserve equal attention, equal care, and a more louder voice.

Credits: Youtube
This Michigan Man Went From 'The Healthiest In The Room' To Battling A Rare AGGRESSIVE Cancer
When Joe Fornasero, a 34-year-old gym buff from Brighton, Michigan, visited the hospital in 2022, he felt he was as healthy as he could possibly be. For over two decades of eating clean and working out consistently, Joe had every reason to think that his healthy habits would keep him safe from chronic disease. But cancer doesn't care about the rules or so it seemed.
Only weeks into his wedding, Joe got a diagnosis so unusual that even veteran oncologists had hardly ever seen a case. He was diagnosed with Desmoplastic Small Round Cell Tumor (DSRCT)—a virulent cancer with fewer than 200 reported cases around the world since it was first discovered in 1989.
Joe's case started out as what appeared to be a routine post-surgical pain. He had just had a hernia repair and during the operation, a benign growth was taken out. Doctors told him the lingering pain and nerve problems were normal.
But the pain in his belly only grew worse. He had chronic stabbing pain in the lower left quadrant and a profound weariness he initially attributed to pandemic stress and career burnout. It wasn't until a physician-friend friend leaned on him to get to the bottom of it that Joe went to the ER. A single CT scan later, his world was turned upside down.
"I went in thinking I was the healthiest man I knew," Joe recalls. "And I came out with a potential diagnosis of cancer."
Misdiagnosis and Medical Whiplash
The initial pathology indicated small cell carcinoma—commonly found with lung cancer. With no time to lose, Joe checked himself into a hospital and underwent chemotherapy. However, something felt amiss.
He was determined to get answers, so he went to MD Anderson Cancer Center in Houston. There, physicians explained the tumors weren't in his lungs. His actual diagnosis came at the eleventh hour in a meeting with a clinical trials specialist. The actual culprit: Desmoplastic Small Round Cell Tumor—a rare and intricate cancer for which no trials were available at the time.
At home, his oncologist admitted to only having studied DSRCT in textbooks. Joe was on his own, dealing with a rare disease that few physicians had experience treating.
Upon finishing six rounds of chemotherapy at Houston, Joe learned his best hope for surgery had disappeared—his MD Anderson doctors had retired. A new hope appeared when he met Dr. LaQuellia at Memorial Sloan Kettering, a top pediatric abdominal surgeon.
The process of removing the tumors was divided into two 10-hour marathons of surgery. The first addressed the upper chest and abdomen—cutting out tumors, lymph nodes, the spleen, part of the diaphragm, and more. Miraculously, Joe was walking 24 hours after surgery.
But the respite was brief. Two cycles of intense chemo followed, along with vicious side effects—nausea, weakness, and mental exhaustion. Then there was the second extensive surgery, where tumors that were still present in his pelvis were removed. This time, Joe heard the words he had struggled so desperately for: remission.
Remission wasn't rest. Joe was aware that the recurrence rate in DSRCT was alarmingly high. He insisted on two more rounds of chemotherapy—despite their debilitating impact—and tolerated whole abdominal radiation that induced extreme gastrointestinal upset and exhaustion.
Maintenance chemo provided some stability, until breathlessness and racing hearts brought another scare. A PET scan showed him to have a one-inch blood clot in his heart. Blood thinners didn't work. Finally, he was diagnosed with early-stage congestive heart failure—a cruel twist in an already agonizing journey.
But Joe never lost hope. A repeat PET scan revealed no evidence of disease (NED). Life appeared to level out for a period. But by mid-2024, a new cause for worry arose. Swollen lymph nodes in his neck caused renewed alarm. Another scan was prescribed, hope and worry by then constant attendants.
Joe's odyssey highlights an essential reality: cancer is indiscriminate. Clean food, running, and strength training cannot entirely protect us from the medical twists of fate that life has in store. His fortitude, tenacity, and self-advocacy embody the resilience of the human condition—and highlight the glaring necessity for more awareness and support for rare cancer patients.
"I figured I was doing everything correctly," Joe says. "But cancer does not care."
His story is more than a personal battle—it’s a call to the healthcare community to invest in orphan disease research, build better diagnostic pathways, and ensure that no patient ever has to hear, “I’ve only read about this in a textbook.”

Credit: Canva
Microplastics Accumulation In Dementia Patients More Than Others, Study Finds
Microplastics are the latest health threat. People across the world have been left worried after recent research found that the accumulation of microplastics in the human brain is equivalent to almost a spoonful. Moreover, there is empirical evidence that shows that these tiny plastic particles can breach the blood-brain barrier that protects the brain from harmful substances.
Measuring how much plastic is in the body is tricky, so there's a lot of uncertainty in that estimate. But the fact of the matter is that scientists have seen these really small, concerning particles in the body. The question is, how harmful are they, really?
What Are Microplastics?
What we know is that plastics are all around us. They're in our furniture, our food supply, our clothes, and cosmetics, and they don't really biodegrade. They just get smaller and smaller in the environment. Microplastics are what result from that. These particles are really tiny, less than five millimeters in size. Because they're so small, they can get everywhere—into our soil, air, into the food chain and into our bodies.
How Are Microplastics Getting Inside Our Bodies?
Researchers at the University of New Mexico found that the primary way these microplastics are getting into our bodies is through ingestion. One notable finding from the lab's research was that the concentration of microplastics in our brains is increasing over time. They showed that from 2016 to 2024, the concentration of microplastics in human brains increased by almost 50%. This increase coincides with the rise of plastic in our world over time. According to some estimates, plastic production doubles every 10 to 15 years.
Do People With Dementia Have Higher Concentration Of Microplastics In Thier Brain?
One particularly concerning finding was that the brains of people with dementia had even more microplastics in them. This could be because the brains of people with dementia are less able to clear out toxins and have a more porous blood-brain barrier. Scientists are trying to figure out causation. Researchers are also investigating the link between microplastics and other health issues like fertility issues, multiple sclerosis, and heart disease.
It will still take years before scientists can actually discover how harmful are microplastics are for our brains. Here are certain things you can do to prevent the threat:
- One is not drinking from plastic water bottles, especially when they've been out in the sun.
- Another is not heating food in plastic containers.
- A third is eating lower on the food chain, so you're not consuming fish and animals that have taken in a lot of microplastics.
© 2024 Bennett, Coleman & Company Limited

