- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Spotting vs Period vs Bleeding: How To Identify
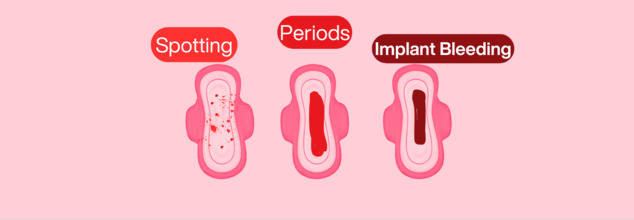
Image Credits: Health and me
A woman's health is intricately linked to her menstrual cycle, which is an important sign of her overall well-being. Throughout puberty and menopause, hormonal changes affect not only fertility but also mood, energy, and long-term health. A normal cycle usually indicates balance, whereas abnormalities may suggest problems such as PCOS, endometriosis, or thyroid disease.
Our bodies do not always work in a perfect clockwork operation and unexpected vaginal bleeding can often confused us. Is it a mere spotting? A normal period? A symptom of something more concerning? Differences between spotting, menstrual bleeding, and intermenstrual bleeding should be understood is crucial for maintaining reproduction health.
Here is a short guide to help you differentiate while you are confused.
Spotting
Spotting is vaginal bleeding that doesn't happen as part of your regular menstrual period. It commonly manifests as fine droplets or smears of blood on clothing or toilet tissue. The intensity of the blood ranges from deep red (recent blood) to pink (having cervical mucus mixed in it) or brown (older, oxidized blood). Spotting is not very much and can't be seen in a way that needs either a tampon or a pad to absorb.
Common Causes of Spotting
Spotting is caused by numerous factors, and in the majority of instances, it is nothing to worry about. Some frequent causes are:
Hormonal Birth Control Transitions: New birth control technique, for instance, birth control pills, IUDs containing hormones, or implants, results in temporary spotting as the body adapts.
Ovulation Bleeding: A few individuals get spotting light around the time of ovulation as a result of hormonal changes. It normally happens in the mid-cycle and could be followed by slight cramping.
Cervical Ectropion: A harmless condition when cells from the inside of the cervical canal migrate to the outer cervix, causing the outer cervix to become more sensitive and prone to faint bleeding on coitus or physical activity.
Early Pregnancy (Implantation Bleeding): 15–25% of pregnant women experience light spotting around 10–14 days post-conception, which is confused with an early period.
When to See a Doctor
Spotting is usually harmless, but it's best to consult a doctor if:
- It continues after a few months of initiating new birth control
- Is accompanied by pelvic pain or abnormal discharge
- Occurs after frequent intercourse
- Occurs during pregnancy and is not verified as implantation bleeding
Menstrual Bleeding
There is a time, also known as a period or menstruation, when the uterine lining sheds due to changing hormone levels. It would last for approximately 2-7 days and is heavier initially. The hue and texture of period blood shift during the menstrual cycle:
Red: New active bleeding at the start of a period
Brown or dark red: Older, slower blood in leaving the uterus
Clots: It's normal to have small clots, but bigger clots may be a sign of heavy menstrual bleeding (HMB)
Why You Have a Period Essentially?
Menstruation is a part of the reproductive cycle, and it happens around every 21–35 days. When there's no pregnancy after ovulation, hormone levels fall, causing the uterine lining to be shed.
Signs Your Period May Be Abnormal
Though periods differ in different people, there are some signs that point towards probable underlying conditions:
- Prolonged bleeding (longer than 7 days)
- Heavy flow necessitating pad/tampon changes every 1–2 hours
- Severe cramps that disrupt daily life
- Irregular periods or absent periods
If you have any of these, conditions such as polycystic ovary syndrome (PCOS), endometriosis, or thyroid disease may be involved, and a medical visit is in order.
Intermenstrual Bleeding
Unlike spotting, intermenstrual bleeding is heavier and unexpected between regular periods. It may be from bright red to dark brown and can contain blood clots.
Possible Causes of Bleeding Between Periods
Sexually Transmitted Infections (STIs): Chlamydia and gonorrhea can lead to inflammation and abnormal bleeding.
Pelvic Inflammatory Disease (PID): A bacterial infection of the reproductive organs and can lead to abnormal bleeding.
Uterine Fibroids or Polyps: Benign growths in the uterus that may cause unexpected bleeding.
Endometrial Hyperplasia or Cancer: In some instances, abnormal bleeding may be a sign of abnormal cell growth in the lining of the uterus.
When to See a Doctor
See a doctor if intermenstrual bleeding is:
- Frequent or persistent
- Associated with pelvic pain or discomfort
- Associated with abnormal discharge, fever or painful sex
Recognizing your body's rhythms can assist you in identifying normal versus abnormal bleeding. Monitoring your menstrual cycle through an app or calendar may flag changes that should be checked with a doctor. If you have any questions regarding abnormal bleeding, visiting your health care provider is the way to go.
US Signs 24 Health MoUs Under ‘America First’ Strategy, More Details Inside

Credits: Wikimedia Commons
The United States has signed 24 bilateral health Memoranda of Understanding or MoUs with Latin America and African countries under the Trump administration's America First Global Health Strategy.
The first agreement with Panama is described as “strengthening Western hemisphere health security”, which it added is “a priority”. Thereafter, four Latin American agreements too involve smaller grants and focus on disease surveillance. Other 20 agreements all with African countries who have been previous recipients of health grants via the now disbanded US agency for International Development or USAID and decimated US President's Emergency Funds for AIDS Relief (PEPFAR).
The five-year MoUs aim to quickly shift financial responsibility for key health services to national governments. In several countries, including Kenya, Uganda and the Democratic Republic of Congo (DRC), more than half of HIV programme funding has traditionally come from donors, particularly the United States. In the DRC, for instance, at least half of the antiretroviral medicines used have been financed by the US.
What Do These MoUs Comprise?
The transitional Memorandums of Understanding (MoUs) signed between the United States and several countries come with a major condition. They require strong investment in infectious disease surveillance systems.
The goal is to ensure that pathogen information from outbreaks is shared with the US within a week. Officials say this helps detect global threats early and protect public health.
At the same time, it gives US pharmaceutical companies early access to pathogen data, allowing them to develop vaccines, medicines and diagnostics more quickly.
The US–DRC Health Agreement
The United States and the Democratic Republic of Congo (DRC) signed their health MoU on 26 February. According to the US State Department, the agreement focuses on strengthening the country’s ability to detect and contain infectious disease outbreaks before they spread internationally.
- The focus reflects the country’s recent health challenges.
- The DRC has experienced several Ebola outbreaks in recent years.
- It is also dealing with the world’s largest mpox outbreak.
Funding Commitments
Under the agreement:
- The US will invest up to $900 million over five years
- The DRC will increase its health spending by $300 million
Most of the funding will support a national integrated surveillance and outbreak response system.
This includes:
- A laboratory network capable of detecting outbreaks within seven days
- Faster outbreak investigations and response systems
- Coordination between the US and other global health partners
The MoU also aims to modernize health data systems through electronic medical records, interoperable platforms, better trained community health workers and expanded services for HIV, tuberculosis, malaria, polio and maternal and child health.
Minerals Before Health
In several cases, health agreements were preceded by deals related to natural resources.
The United States and the DRC first signed a strategic partnership on critical minerals. The deal aims to secure supplies of minerals needed for commercial and defense industries.
The DRC is one of the world’s largest sources of rare earth minerals, including cobalt and copper. China has historically dominated the purchasing and processing of these resources.
Recently, the DRC has begun opening its mineral sector to US investors. According to Reuters, the government sent Washington a shortlist of state owned assets involving:
- manganese
- copper
- cobalt
- gold
- lithium
Guinea followed a similar path. It signed a minerals MoU with the US on 5 February, followed by a health MoU on 27 February. The health agreement prioritizes strengthening laboratory networks and improving biosafety standards by 2027.
Legal Pushback and Rejected Deals
Not all countries are comfortable linking health support to access to resources or data.
In the DRC, a group of lawyers has challenged the minerals agreement in the Constitutional Court. They argue that the deal violates the constitution and undermines national sovereignty over natural resources.
Zimbabwe also withdrew from negotiations with the US over a similar agreement.
Officials said the country was asked to share biological resources and outbreak data for years without any guarantee that vaccines, treatments or diagnostics developed from that data would be available to Zimbabwe if a future crisis occurred. They also said the US did not offer reciprocal sharing of its own epidemiological data.
Concerns in Kenya and Zambia
Kenya’s agreement with the United States has also faced legal hurdles. The country’s High Court halted the MoU after two court challenges questioned provisions that could allow the US access to patient data and pathogen information.
Zambia has also expressed reservations about its proposed health deal with Washington. The agreement stalled after the US linked the billion dollar package to cooperation in the country’s mining sector, particularly copper and cobalt.
Zambia has since asked for revisions, saying parts of the deal do not align with its national interests.
Critics Call the Policy “Extractive”
Some experts argue that these agreements reflect a broader shift in US global health policy.
Sophie Harman, professor of international politics at Queen Mary University of London, wrote in the BMJ that extraction appears to be central to the approach.
According to her analysis, the policy focuses less on improving global health outcomes and more on strengthening US economic and geopolitical interests, including competition with China.
She warns that countries entering such agreements could risk giving up resources or scientific data while gaining relatively limited health benefits.
Digital Health and Telemedicine: Expanding Access to Rare Disease Care

(AI Generated)
Rare diseases may be individually uncommon, but together they represent a large and persistent care gap. More than 300 million people globally live with a rare condition, and when families and caregivers are counted, the impact touches over one billion lives. The economic burden is estimated to exceed $7 trillion each year.
In India, the challenge is compounded by geography, uneven specialist availability and the lifelong nature of many rare conditions. The question is no longer whether the system recognises the need, but whether it can deliver continuous care at scale.
Why Patients Still Struggle To Reach Care
For most rare disease patients, the hardest part is not always the science but the pathway to care. Diagnosis is often delayed, sometimes by years. Patients move between providers carrying incomplete records. Specialist centres are concentrated in a few large cities, forcing families to travel repeatedly for consultations that may last only minutes. This is both financially draining and clinically inefficient.
Telemedicine is beginning to ease some of this pressure. Virtual consultations allow specialists to extend their reach beyond metropolitan clusters. For families in tier two and tier three locations, this can mean earlier clinical input and fewer avoidable journeys.
Remote monitoring tools are also shifting care from episodic hospital visits to continuous oversight, which is particularly valuable for conditions that require close tracking over time.
Why Data Matters More Than Ever
If access is the visible challenge, data fragmentation is the structural one. Rare disease information remains scattered across hospitals, laboratories and individual case files. This weak visibility affects everything from prevalence estimates to therapy development. Policymakers struggle to size the problem accurately. Clinicians miss longitudinal patterns. Industry investment becomes harder to justify.
Digital health systems can address this by creating longitudinal patient records that follow individuals across providers. Even relatively modest steps such as strengthening diagnostic reporting or building disease registries can significantly improve coordination. For rare diseases, where patient numbers are small and widely dispersed, structured data is not a luxury. It is the backbone of effective care.
India’s Digital Opportunity
India has begun building the rails needed for this transition. The Ayushman Bharat Digital Mission is creating a national health data architecture anchored in unique health IDs and interoperable records. If applied rigorously to rare diseases, this infrastructure can support lifelong patient tracking, improve referral accuracy and give policymakers clearer visibility into disease burden.
Interoperability will determine how far this effort goes. The growing adoption of FHIR standards and API led systems is slowly allowing previously disconnected hospital platforms to exchange clinical information. For rare disease patients, whose care often spans multiple providers and years of follow up, this continuity is not technical detail. It is essential to safe treatment.
AI Moves From Promise To Practice
Artificial intelligence is also starting to show practical value. Globally, AI based clinical decision support tools are being used to flag potential rare disease cases hidden within routine health records. This matters because many rare conditions present with non specific symptoms and are frequently missed in early stages.
Collaborations between technology firms and pharmaceutical companies are demonstrating how electronic health record analysis, suspect patient lists and longitudinal data can help clinicians triage cases earlier for confirmatory testing. As these tools mature and integrate into routine workflows, they could significantly shorten the diagnostic odyssey that rare disease families currently endure.
Engaging Patients Beyond The Clinic
At the patient level, the shift is becoming more practical and visible. Tools that let people log symptoms, get medication reminders and share updates in real time are helping them stay more consistent with treatment, while giving clinicians better insight between visits. For lifelong conditions, this kind of day to day support brings care into the flow of everyday life, where most disease management actually happens.
Federated data models add an important layer of trust. By enabling analysis across multiple small patient populations without moving sensitive personal data, they address both privacy concerns and the sample size limitations that have historically slowed rare disease research.
From Pilots to Systems
Progress is visible across both public and private sectors. Regulated digital health platforms are already supporting rare disease programmes in several countries. Industry collaborations are using AI to detect conditions that often go undiagnosed for years. Public genomic databases are generating new diagnoses by enabling experts to build on shared evidence.
India’s immediate task is to move beyond isolated pilots. Telemedicine networks must be tied to referral protocols and reimbursement pathways. Digital registries must be built with strong governance and patient trust. AI tools need to be embedded into everyday clinical workflows rather than remaining demonstration projects.
Why Investment Makes Fiscal Sense
Poorly managed rare diseases create avoidable hospitalisations, lost productivity and long term care costs. Evidence increasingly shows that targeted investments in data systems, screening and coordinated care can reduce downstream expenditure. For low- and middle-income countries working within tight health budgets, these are not marginal gains.
India already has many of the building blocks needed to improve rare disease care, from expanding digital health infrastructure to growing AI capabilities and increasing policy focus. The real test now is disciplined execution.
Telemedicine networks must deepen their reach, patient registries need to become reliable and usable, data must move securely across systems, and clinicians should have decision support tools that fit into everyday practice. Taken together, these steps can meaningfully narrow today’s access gaps.
Digital health will not make rare diseases any less complex. But if implemented thoughtfully, it can reduce distance, shorten delays and bring much needed continuity to care journeys that are currently fragmented. For families managing lifelong conditions, that would be a tangible and much overdue shift.
When Symptoms Don’t Add Up: How Hidden Genetic Conditions Go Undetected for Years

(AI Generated)
In India, it is not uncommon for families to travel across cities, sometimes across states, seeking answers for symptoms that simply don’t make sense. A child who is not meeting developmental milestones. A young adult with unexplained muscle weakness. Recurrent hospital visits with no clear diagnosis.
For many, this long and frustrating search for clarity is what medicine calls the diagnostic odyssey.
Rare diseases are individually uncommon, but collectively they affect millions of people worldwide. Rare diseases affect an estimated 263–446 million people worldwide, spanning every geography, healthcare system, and socioeconomic context. India alone is estimated to have 70 million people living with rare diseases.
Importantly, although 70%–80% of rare diseases are genetic in origin, routine medical practices often consider genetic testing only after years of inconclusive evaluations.
In India, this challenge is amplified by several factors, including limited awareness of rare conditions, uneven access to specialized testing across regions, and a tendency to treat symptoms individually rather than look for a unifying cause.
A child may see a neurologist for seizures, a gastroenterologist for feeding issues, and a developmental pediatrician for delays, without anyone connecting the dots.
Studies have shown that patients and their families frequently wait years before receiving a confirmed diagnosis. Globally, rare disease diagnosis can take anywhere between 5–30 years.
In a country like India, where healthcare expenses are often paid out-of-pocket, this prolonged uncertainty can be devastating. Beyond cost, there is the psychological toll; parents wondering if they missed something and adult patients often questioning whether their symptoms are “all in their head”. During this period, families undergo repeated tests, face conflicting opinions, and bear significant emotional and financial strains.
Research shows that families experience profound emotional burden during the diagnostic odyssey, including stress, anxiety, and feelings of isolation.
Why Do These Conditions Stay Undetected For Years?
In many cases, the explanation is written into a person’s DNA. Genetic disorders rarely announce themselves clearly; instead, they often mimic common illnesses. Fatigue may look like anemia, developmental delay may resemble a learning difficulty, and repeated infections might be treated as isolated events rather than part of a larger pattern. Because the symptoms overlap with more familiar conditions, doctors naturally begin by treating what appears most likely.
Most healthcare systems also follow a step-by-step diagnostic approach; rule out the common causes first, then move to less common ones if symptoms persist. While this method works well for typical illnesses, it can significantly delay answers for rare genetic conditions. Without looking directly at the genetic blueprint, the underlying cause may remain hidden, even as the visible symptoms are managed one at a time.
Today, advances in genomic technologies such as whole-exome sequencing (WES) and whole-genome sequencing (WGS) allow us to examine thousands of genes simultaneously. Rather than guessing which gene might be responsible, we can comprehensively analyze a patient’s DNA to search for answers.
Evidence increasingly supports the use of genomic sequencing earlier in the diagnosis and care of rare diseases. Similarly, studies highlight how genomic testing not only provides diagnoses but also directly influences treatment decisions and long-term care planning.
In the Indian context, integrating genetic testing earlier could transform care. Instead of years of fragmented consultations, patients could receive a precise diagnosis sooner. This clarity can:
- Prevent unnecessary or repeated investigations
- Guide appropriate treatment strategies
- Inform family members about potential risks
- Enable informed decisions about future pregnancies
- Equally important, it replaces uncertainty with understanding.
Encouragingly, awareness around rare diseases is growing in India, and conversations around early genomic testing are becoming more mainstream. As technology becomes more affordable and accessible, we have an opportunity to fundamentally change the patient journey.
No family should spend years searching for answers when science has the tools to help. By embracing genomic medicine earlier in the diagnostic pathway, we can shorten the odyssey, reduce suffering, and empower families with clarity.
Because when symptoms don’t add up, sometimes the answer lies written in our genes.
© 2024 Bennett, Coleman & Company Limited

