- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Should You Take Cryotherapy? Know It's Benefits And Risks

Cryotherapy (Credit: Canva)
Cryotherapy is a modern-day treatment wherein the body is subjected to extremely cold temperatures for several minutes. You can just get one part of your body exposed to (localised cryotherapy) and opt for whole-body cryotherapy. The first can be done in several ways like through ice packs, ice massages, coolant sprays, ice baths and even through probes administrated into tissue. A lesser-known fact is that the use of low temperature in healing dates back to 2500 BC. However, it only came into modern practice after being used by Japanese doctor Yamaguchi in 1978 to treat people with rheumatoid arthritis.
How Does This Treatment Work?
The theory for whole-body cryotherapy (WBC) is that by immersing the body in extremely cold air for several minutes, you could receive a number of health benefits. Throughout the process, the individual stands in an enclosed chamber or a small enclosure that surrounds their body but has an opening for their head at the top. The temperature in the enclosure drops to between negative 200–300°F. The person stays in the ultra-low temperature air for between two and four minutes.
You can get benefits from just one session of cryotherapy but it is most effective when used regularly. There are many athletes who do this regularly, some athletes use cryotherapy two times every day and others will go daily for 10 days and then once a month afterwards.
Key Benefits Of Cryotherapy
1. Relieves Migraine Symptoms: Cooling the neck's carotid arteries helps reduce pain by cooling blood in intracranial vessels.
2. Eases Nerve Pain: Cryotherapy numbs irritated nerves, aiding in the treatment of pinched nerves, chronic pain, and acute injuries.
3. Improves Mood: By triggering hormonal releases like endorphins, it may help alleviate anxiety and depression.
4. Reduces Arthritic Pain: Whole-body cryotherapy can minimize arthritis pain and enhance rehabilitation.
5. Aids Cancer Treatment: Targeted cryotherapy ("cryosurgery") freezes and kills cancer cells in low-risk tumours, like prostate cancer.
6. Supports Cognitive Health: Its anti-inflammatory effects may prevent Alzheimer’s and dementia, though research is ongoing.
7. Treats Skin Conditions: Conditions like atopic dermatitis and acne may benefit from reduced inflammation and improved antioxidant levels.
What Are The Risks Of This Treatment?
Cryotherapy is not suitable for people with nerve-related conditions or diabetes due to the risk of further nerve damage. Many can face side effects such as temporary numbness, redness, and skin irritation. To ensure a safe session, limit sessions to four minutes in whole-body cryotherapy chambers. Avoid applying ice directly to the skin or for more than 20 minutes. Another important measure one should take is always to consult a healthcare provider before starting cryotherapy, especially for medical conditions.Cryotherapy has a beneficial impact on your mental health too. Experts say that cryotherapy has the potential to effectively treat stress disorders like general anxiety, depression Post-traumatic Stress Disorder (PTSD), and Obsessive Compulsive Disorder (OCD.)
A 2012 study also suggested that cryotherapy can mitigate inflammation and oxidative stress, which is linked to dementia, mild cognitive impairment other age-related cognitive decline. Another study conducted in 2008 found that cryotherapy reduced symptoms by at least 50% in one-third of individuals with depression or anxiety.
Reducing Mother-To-Child HIV Transmission To Zero Key To End AIDS In India: Experts

Credit: iStock
Reducing mother-to-child HIV transmission, also called vertical transmission, to zero is crucial to achieve the end AIDS target by 2030 in India, in line with the UN Sustainable Development Goals, said experts.
At the 17th National Conference of the AIDS Society of India (ASICON 2026), health officials and experts together deliberated on the progress made in the country against HIV and also called for a stronger last-mile effort to eliminate AIDS from the country.
While India has made a major reduction in vertical HIV transmission, with just 0.7 percent of infant diagnoses. But the experts stressed the need to further reduce it to zero.
From 25 percent in 2020, the vertical transmission of HIV has come down to 11.75 percent in 2023, according to Dr. Glory Alexander, President of AIDS Society of India (ASI).
“Before treatments were available to prevent vertical transmission, the risk of a newborn acquiring HIV in India ranged from 15 percent to 45 percent. The risk was nearly 45 percent among infants who were breastfed,” Dr. Alexander said.
She attributed the reduction to the introduction of antiretroviral therapy (ART) and implementation of HIV prevention and treatment guidelines.
"The government has successfully reduced the rate of infant HIV diagnosis (risk of a child getting infected with HIV due to vertical transmission) to 0.71 percent. We need to further reduce it to zero to eliminate vertical transmission of HIV,” Dr. Alexander added.
Intensifying Last-Mile Approach
India reportedly has 27-29 million pregnancies every year.
As per the latest National AIDS Control Organization (NACO) report, 83 percent of all pregnant women are tested for HIV, and 78 percent of all pregnant women are tested for syphilis in India.
“Out of an estimated 19,000 pregnant women who might be living with HIV in India, over 16,000 were reached by the government-run program and linked to services -- half of them were newly diagnosed with HIV,” Dr. Alexander said.
NACO runs 794 antiretroviral therapy centers across the country and provides free HIV treatment to 18 lakhs people with HIV.
NACO's over 700 “Suraksha Sewa Kendras” also provide preventive services for people who are at risk of acquiring HIV.
Dr. Ishwar Gilada, Emeritus President of AIDS Society of India (ASI), called India's progress "commendable."
"But to end AIDS, the last mile approach has to be accelerated and intensified manifold,” the expert said.
Increase HIV Testing Manifold
Dr. Gilada stressed the need to "ensure that all key populations know their status, and those with HIV are linked to treatment, care, and support services and remain virally suppressed".
If a person with HIV is virally suppressed, then there is zero risk of any further HIV transmission, as per the WHO, he added.
Indian data shows 9-43 times higher HIV rates (as compared to the general population) among key populations, such as men who have sex with men, transgender people, sex workers, people who inject drugs, among others.
These key populations are hard to reach, which warrants community-led and science-backed approaches, said Dr. Gilada.
Reducing Advanced HIV Disease
Despite commendable progress in India’s HIV response, there is a huge number of cases of advanced HIV disease (AHD) -- about one third of all people living with HIV in the country, the experts said.
The World Health Organization (WHO) defines AHD as a CD4 count less than 200 cells per cubic millimeter/ or WHO stage 3/4 in adults/adolescents, and all children less than 5 years old.
It indicates a severely weakened immune system, high mortality risk, and vulnerability to infections like TB and cryptococcal meningitis.
AHD cases in India are majorly among those who are HIV infected but are not on lifesaving antiretroviral treatment.
"This could be because HIV infection is undiagnosed in people until they present with opportunistic infections to healthcare centers, or they were not able to adhere to the treatment for a range of reasons,” said Dr Trupti Gilada, Joint Secretary, AIDS Society of India (ASI).
TB, which is preventable and treatable, is the most common opportunistic infection among people with HIV.
Another concern is the rising antimicrobial resistance in HIV patients. Studies show that people with HIV are 2-3 times more likely to get drug-resistant forms of TB.
Romanticization And The Silent Dismissal Of Women’s Pain | Women's Day Special

Credits: Canva
Just few days ago, the world witnessed a personal documentary film bagging BAFTA Award 2026. The film is titled This Is Endometriosis. The film is a personal story of director Georgie Wileman, who was diagnosed with the condition a decade after she had first shown her symptoms. The film brings the attention back on dismissal of women's pain, which has been normalized for ages.
This is not the only instance of women's pain being dismissed. Instagram and other social media platforms are flooded with women sharing their experiences of getting intrauterine contraceptive device or an IUD inserted without anesthesia. The pain is debilitating.
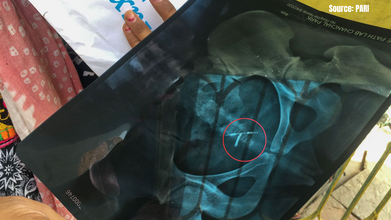
Another report, from India's capital city by PARI (People's Archive of Rural India) mentions a case of Deepa (name changed) who had a copper-T (IUD) inserted, right after her C-section. After two years, she experienced menstrual irregularities and heavy bleeding. She visited several doctors, one of whom, even dismissed it as just weakness, while prescribing calcium and iron tablets for her. In other instances, her copper-T could not be located, until she got an X-ray done, which noted: 'The copper-T is seen in situ in hemipelvis region.' The PARI report quotes West Delhi-based gynecologist Dr Jyotsna Gupta, "There are high chances that a copper-T may get tilted if it is inserted soon after delivery or a C-section.This is because in both cases the uterus cavity is enlarged then, and takes time to set itself to normal. While it is doing so, the inserted copper-T may change its axis and get tilted. It may also get displaced or get tilted if a woman experiences severe cramps during menstruation.”
The report also quotes ASHA worker Sushila Devi saying that they hear many women complaining about copper-T. "Many times, they tell us that it has 'reached their stomach' and they want to get it removed." However, like this case, in many other cases too, their pain is often ignored.
When Health and Me spoke to Dr Archana Dhawan Bajaj, gynecologist and Delhi-based IVF specialist, she said that physical pain and emotional distress in women is often normalized because the system "assumes that women's bodies are always in a state of flux and therefore leads to many women being undiagnosed or dismissed and delayed for treatment of a serious nature."
Dr Sonu Taxak, who is a senior IVF Consultant and Director at Yellow Fertility also told Health and Me that historically, women's symptoms were poorly studied, so for any pain, "hormonal fluctuation became a convenient explanation".
Read: The Hidden Cost of Extreme Fitness On Women’s Bodies | Women's Day Special
Women Bodies Are Meant To Bear Pain
A popular monologue from Fleabag says, "Women are born with pain built in." The powerful monologue is a reminder of how women carry pain and are often unheard so much so that society makes a woman believe that she is meant to bear it. While there is no scientific evidence that verifies that women have a higher pain tolerance than men (British Journal of Anaesthesia, 2013), historically their pain have been ignored. Dr Taxak points out that research consistently shows women’s pain is more likely to be dismissed as emotional or anxiety-related. "While awareness is improving, unconscious bias still exists. Pain should be evaluated based on clinical evidence, not gender-based perception."
A Guardian report from 2020 talks about how women are shamed for asking for painkillers. The report mentions Kate, who was in a 26-hour labor and when she asked for epidural, she was denied it. "The first time the midwives said I wasn't far enough along. The second time, they said I didn't need it. Finally, they said I was too far along."
Many women are shamed for asking for epidural, or are often scared. Yashasvi Arora (name changed) delivered her baby in January 2025 in a Delhi hospital said that her mother had told her to not opt for epidural as it causes chronic back problems that linger throughout one's life. However, science finds no such evidence of any claim. While back pain is common, but it does not stay forever, as notes Cleveland Clinic.
"Childbirth pain has been culturally romanticized as something to 'endure'. But medically, an epidural is a safe and evidence-based pain relief option. Choosing comfort does not diminish strength, It reflects informed decision-making," says Dr Taxak.
Pop culture plays a significant role in romanticization of labor pain. An advertisement by Indira IVF opens with a woman in labor pain, sweating and screaming and in the next scene, she says, "This is my life's best moment". Dr Archana says, "Pain relief (i.e., epidurals) becomes defined as a form of weakness because society favors natural childbirth as a true "test of endurance." Additionally, society often manifests culture as a glorified sacrifice made by the mother and that to ask for help is a sign of failure."
The cycle of pain does not end there, women are also shamed for postpartum, with many, especially men on the internet claiming that it is not a real thing. A new trend of 'Last Generation of the Innocent Mother' has taken over the internet that glorifies mothers who did not express their problems or were often shamed for it. However, the reality is quite different from what trends on the internet.
Read: Navigating Postpartum: The Emotional and Physical Impact on New Mothers
“I am a very positive person. I know I can handle anything. So, when my friends would tell me their stories of postpartum, I would tell myself that I could handle it. I could talk myself out of it. But to my surprise, it was very difficult. My body and my mind went through so much,” says Akanksha Thapliyal, 34 from Siliguri, a creative consultant, who became a mother at 33. Thapliyal shares that there were days when she would just cry, without even knowing the reason. At times, everyone felt like her enemy, including her husband.
A mother from East Tennessee, Tiffany Toombs Clevinger, now 39, shares she was 37 when she had her baby and her first feeling was, “Oh no, what did we just do?” She was in disbelief and did not know what to do to take care of her child.

Both mothers struggled with breastfeeding and Thapliyal also complained of pain while feeding her child. However, her mother told her that it was normal. The reality is, it was not.
"Postpartum depression is often underdiagnosed because symptoms are normalized or overlooked. While mild discomfort in breastfeeding could occur initially, persistent or severe pain is not normal," points out Dr Taxak.
Pain And Discomfort Exist Only For Men
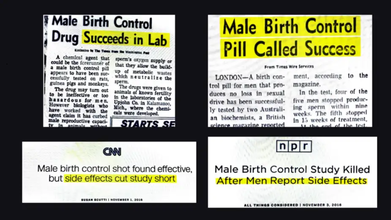
Birth control pill is often the burden on women, and when the idea of male contraception was first discussed in 1970s, the research came to a halt. The pill never made it to market. In November 2016, Susan Scutti reported in CNN that the study was cut short due to the side effects of the pill. The report Male birth control shot found effective, but side effects cut the study short. Another report by NPR titled Male Birth Control Study Killed After Men Report Side Effects also seconded the claim.
Read: Explained: The History Of Birth Control Pills And Other Alternative
While for women, those who are on birth control pills are prone to headaches, breast tenderness, acne, nausea, weight gain, irregular menstruation, mood changes, and decreased libido.
Dr Archana explains, the disparity of how women and men are treated medically in terms of contraceptive responsibility remains pervasive due to long-standing societal and medical expectations. "Trials for male contraceptives are often stopped due to the mildly adverse effects of men, while women have been expected to suffer similar or perhaps even more serious effects for a much longer period. Ultimately this further illustrates the gendered tolerance men have witnessed in the medical world, wherein the discomfort of women is often treated as 'the norm,' while any form of adverse side effect for men exhibits heightened scrutiny and ultimately leads to decisions to cease the trials."
Listening To Women's Pain
With such instances, it becomes more so important on International Women's Day on how much of women's pain is still being normalized instead of treated. For decades, medicine and society have often asked women to tolerate discomfort quietly.
International Women’s Day, at its core, is about recognizing women’s voices and experiences. In healthcare, that means something very practical: believing women when they say something is wrong. Because sometimes, the most powerful step toward better care is not a new technology or treatment. It is simply listening.
How Is Today's Lifestyle Impacting Childhood Obesity in India? An Expert Explains

Credits: iStock
Childhood obesity is rapidly emerging as one of the most serious public health concerns across the world, and in India too. Once considered a problem limited to adults, excess weight is now affecting children at younger ages and increasing their risk of chronic diseases early in life.
According to The World Obesity Atlas 2024 by the World Obesity Federation, India ranks second globally in the number of children living with overweight and obesity, just behind China. The report estimates that out of 56 million children affected in the country, around 20 million are likely to be obese, while the rest are expected to fall in the overweight category.
Read: Childhood Obesity In India To Surge To 56 Million By 2040, Says Global Report
The situation is not limited to India. Globally, the number of children aged 5 to 19 years living with overweight or obesity is projected to reach 507 million by 2040, rising sharply from 419 million in 2025.
Experts say the rise is closely linked to how children eat, move, and spend their time today.
Childhood Obesity Is More Than A Cosmetic Issue
Dr Ruchi Golash, Pediatrician at CK Birla Hospitals, CMRI, explains that childhood obesity goes far beyond appearance and can have long-term health consequences.
“Excess weight in childhood is not just a cosmetic concern. It significantly increases the risk of conditions such as diabetes, high blood pressure, fatty liver disease and early heart problems,” she says.
Read: 1 In Every 8 School-going Children Is Obese In Kolkata: Study
Children who develop obesity early in life are also more likely to remain obese as adults if the issue is not addressed in time. This makes early prevention and lifestyle changes especially important.
The Role Of Excessive Screen Time
One of the biggest lifestyle changes affecting children today is the rise in screen time. From online classes and gaming to streaming videos, children are spending several hours each day in front of screens.
Dr Golash notes that this shift is contributing significantly to weight gain.
“Prolonged screen use reduces physical activity, disrupts sleep patterns and often encourages mindless snacking,” she explains.
Exposure to screens, especially before bedtime, can also interfere with hormones that regulate hunger and fullness. As a result, children may feel hungrier and eat more than their bodies need.
Ultra-Processed Foods Are Becoming The Norm
Another major factor behind rising childhood obesity is the shift in dietary habits.
Ultra-processed foods such as packaged snacks, sugary beverages, instant noodles and bakery products have become widely available and heavily marketed to children. While convenient and appealing, these foods are typically high in calories, sugar, salt and unhealthy fats.
“They are low in fibre and essential nutrients, which means children consume a lot of energy without getting adequate nutrition,” Dr Golash says.
Regular consumption of these foods can lead to rapid weight gain, insulin resistance and early metabolic problems, increasing the risk of long-term health complications.
Decline In Outdoor Play And Physical Activity
Sedentary lifestyles are another key contributor. Compared to previous generations, children today spend far less time playing outdoors.
Academic pressure, safety concerns and the lure of digital entertainment have gradually replaced active play with more sedentary activities.
“Even children who do not overeat can gain weight if they are not physically active enough,” Dr Golash explains. Reduced muscle activity slows down metabolism and allows fat to accumulate more easily in the body.
What Parents Can Do To Prevent Childhood Obesity
Experts say parents play a central role in preventing childhood obesity and helping children build healthier habits.
Dr Golash advises families to start with simple lifestyle changes such as limiting daily screen time, encouraging outdoor play and prioritizing home-cooked meals.
“Setting reasonable screen-time limits, promoting daily physical activity and reducing sugary drinks can make a significant difference in a child’s overall health,” she says.
She also emphasizes that conversations about weight should focus on healthy habits rather than appearance.
Early and supportive interventions, she adds, can help reverse unhealthy weight gain and protect a child’s long-term heart and metabolic health.
© 2024 Bennett, Coleman & Company Limited

