- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
8 Twisting Yoga Poses You Should Do For Spinal Health

(Credit-Canva)
Yoga has many aspects to it, whether it is muscle health, bone health, mental health etc. Not only does it help us improve the physical functions of our body, but it also helps us enhance our well-being. Many studies have shown the benefits of it; trainers and healthcare professionals alike encourage people to practice it regularly. There are many different types of yoga poses, there are poses that focus on your muscle flexibility, enhancing organ function like lungs, as well as strengthening your bones like your spine.
According to the International Journal of Yoga, twisting poses squeeze out old blood from your organs, letting fresh, oxygen-rich blood flow in when you release the twist. Yoga boosts blood flow and increases hemoglobin and red blood cells. This means more oxygen gets to all your body's cells, helping them work better. Yoga can also thin your blood, which may lower your risk of heart attack and stroke, as these are often caused by blood clots.
Twisting Yoga Poses You Should Try
Easy Supine Twist (Supta Matsyendrasana)
This is a gentle warm-up twist that feels great. It helps lengthen your spine, open up your ribs, and gently awaken your core muscles. It's a perfect way to start any yoga twist sequence. Simply lie on your back and follow the steps to gently twist your body.
Twisting Down Dog (Parivrtta Adho Mukha Svanasana)
Add a twist to your usual Downward-Facing Dog. This pose gets your body ready for deeper twists and specifically targets your middle back. You'll shift your weight and reach one hand back to twist your upper body, looking under your armpit. Remember to keep your hips level for the best twist.
Plank Twist Knee-to-Elbow (Phalakasana Variation)
Do a few of these to really wake up your core. This pose helps your core muscles become strong and stable, which is super important for supporting your spine in more intense twists later on. You'll move from a three-legged dog, bringing your knee towards your opposite elbow.
Revolved Chair (Parivrtta Utkatasana)
To get the most benefit from this pose, make sure your knees and hips stay in line. This helps ensure that the twisting action happens mainly in your middle back and neck, rather than straining your lower body. Sit back as if in a chair, bring your hands together, and then twist.
Revolved Lunge (Parivrtta Anjaneyasana)
This straightforward twist is excellent for warming up your entire body. From a lunge position, you'll rotate your chest towards the sky, creating a long line from your grounded hand to your lifted fingertips. It's a great way to build heat and mobility.
Revolved Triangle (Parivrtta Trikonasana)
This is a more challenging twist that needs a lot of practice and flexible hamstrings. You'll stand in a wide stance and twist deeply, trying to bring your hand across to the outside of your opposite foot. Take your time with this one and remember to breathe.
Revolved Pyramid (Parivrtta Parsvottanasana)
Also known as Intense Side Stretch, this twist is quite similar to Revolved Triangle but has a slightly different stance and hand placement. You'll hinge forward from your hips with a flat back, then twist your upper body open, extending one arm to the sky.
Revolved Half Moon (Parivrtta Ardha Chandrasana)
This pose combines a deep twist with a balance challenge. You'll start in Warrior 3 and then twist your upper body open while balancing on one leg. It's a tough but rewarding pose that builds strength and stability.
India For The First Time Has Guidelines On Muscle Loss
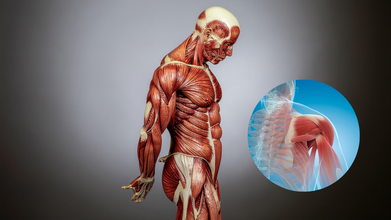
Credits: Canva
Mobility and independence are two things that keep people healthy, however, with age, as bones weaken and muscle is lost, elderly become more dependent. This condition is called sarcopenia, or age-related muscle loss. India is finally focusing on this and have now new guidelines to warn people against it.
The Geriatric Society of India released country's first 'Indian Guidelines for the Evaluation and Management of Sarcopenia'. These guidelines are a combination of recommendations by experts across multiple specialties, including geriatric medicine, orthopedics, endocrinology, physiotherapy and nutrition. These guidelines aim to help doctors detect and treat muscle loss early. The aim is to not let elderly compromise with their independence.
Also Read: Bruce Willis Health Update: His Death News Is A Hoax; 'He's Still Alive And Well'
What Is Sarcopenia?
Sarcopenia literally translates to 'loss of flesh'. Medically, it refers to gradual decline in muscle mass, strength and physical function with aging. While it is often overlooked, it is also the major reason for many fractures and hospitalizations of older adults, and sometimes, even death.
India is expected to have around 319 million people aged over 60 by 2050, which is one-fifth of the population. It could be concerning as they are at risk of sarcopenia. Studies have also shown that the number has increased from 8-18 per cent to 25-40 per cent adults, especially hospitalization cases. Experts point out that those with chronic diseases like diabetes are at a higher risk.
What Are The First Indian Guidelines On Muscle Loss or Sarcopenia?
Dr OP Sharma, who led guidelines said that muscle health is most important for healthy aging. "Strength preserves dignity. Early detection saves independence," he said. Dr Sharma also noted that the sedentary lifestyle, poor nutrition and chronic illnesses are accelerating this condition among seniors.
The guidelines also advise doctors to look for warning signs in patients, which include weak grip strength, slower walking speed, or difficulty getting up from a chair. There are also screening tools like SARC-F questionnaire, which could help identify those at risk.
The ray of hope here is that sarcopenia could be prevented or slowed that too with simple lifestyle changes.
What Lifestyle Changes Could Prevent Sarcopenia?
- Strength training exercises
- Adequate protein consumption
- Correcting deficiency including vitamin D and calcium
Doctors are also advising to eat a balanced diet, which includes protein, fats, green vegetables, and pulses. Dr Raju Vaishya of Indraprastha Apollo Hospitals said, "India is a sarcopenic nation". He pointed that everyone needs to be aware about muscle health, however this awareness remains low in the country.
Dr Randeep Guleria said the guidelines aim to brings muscle health into routine medical care. "They bridge science with clinical wisdom, making sarcopenia visible in everyday practice."
Can Just 10 Minutes of Exercise Reduce Depression?

Credit: Canva
A new Nature Human Behaviour (2026) study suggests that single-session psychological exercises lasting less than 10 minutes can lead to measurable decreases in depression symptoms even one month later.
Depression is one of the most common mental health disorders in the world. Every year, hundreds of millions of people suffer from depression, and many are unable to get therapy because of cost, stigma and the dearth of mental-health professionals.
Symptoms include excessive sadness, depression often includes fatigue, changes in appetite, sleep disturbances, difficulty concentrating and feelings of hopelessness. Treatment requires professional guidance for diagnosis and management.
A 10-Minute Intervention With Lasting Effects
Researchers conducted one of the largest randomized controlled trials testing short mental-health exercises and recruited 7,505 adults in the United States who were suffering from symptoms of depression and randomly assigned them to one of several short digital interventions or to a control group.All the brief interventions took less than 10 minutes to complete and were designed to teach practical coping skills that are commonly used in psychotherapy. Some exercises helped participants to reframe negative thoughts, while others focused on motivation, goal-setting or making sense of things by helping others. Participants completed surveys measuring their well-being immediately after the session and again one month later.
The results were striking: while many exercises boosted motivation and hope immediately, two interventions - Interactive Cognitive Reappraisal and Finding Focus - showed measurable reductions in depression symptoms even after a month. On average, participants experienced about a four percent greater reduction in depression scores compared with the control group.
Although the improvement may appear small, researchers note that brief, scalable interventions could reach millions of people who currently lack access to mental-health care as they can be completed in a few minutes and delivered online, these exercises may allow people to take initial steps toward better mental health, especially those waiting for professional help or unwilling to ask for help.
The scientists also stressed that these activities are not intended to substitute for therapy, but should be seen as readily available tools to help with emotional health.
Exercise and Mental Health: A Growing Body of Evidence
Previous research also shows that a quick burst of activity can make you feel better from other research too. A British Journal of Health Psychology 2024 study found that just 10 minutes of daily mindfulness practice significantly improved well-being and reduced symptoms of depression and anxiety among more than 1,200 participants from 91 countries.
Similarly, the US National Institutes of Health (2019) reviews suggest that the physical activity itself may help improve mood and depressive symptoms, strengthening the relationship between movement and mental health.
Collectively, these findings suggest that even small doses of mental or physical activity may lead to psychological benefits.
A Small Step That Can Make a Difference
Depression can make people feel trapped and out of control. The good news of the new research is that it suggests that big changes aren’t always necessary to move forward.
Sometimes, doing a small task, like spending 10 minutes learning a new coping skill or doing a quick mental exercise, is enough to change the way you think and gradually improve mood.
As researchers investigate these brief interventions, one thing is becoming clear: when it comes to mental health, few minutes matter more than we think.
Can Too Much Running Worsen PCOS? Gabby Logan Opens Up About Athlete Daughter’s Diagnosis

Credits: Instagram
British broadcaster Gabby Logan has revealed that her 20-year-old daughter Lois has been diagnosed with polycystic ovary syndrome (PCOS), a hormonal condition that may require her to step back from high-intensity endurance sport, including extreme long-distance running.
Speaking on her Mid-Point podcast, Logan said the diagnosis came after medical consultations about her daughter’s health and training. During the appointment, a specialist advised Lois to avoid “extreme running,” prompting mixed emotions in the family, concern about the condition, but also relief about scaling back punishing physical goals.
What PCOS Means for Athletes
PCOS is one of the most common endocrine disorders in women of reproductive age, affecting an estimated 8–13 per cent globally. It occurs when the body produces higher levels of androgens (male-type hormones) and often involves insulin resistance.
The condition can cause irregular periods, acne, excessive hair growth, weight changes and fertility challenges. Many patients also have difficulty regulating blood sugar, increasing long-term risks of type 2 diabetes and heart disease.
While exercise is widely recommended as a cornerstone of PCOS management, helping improve insulin sensitivity, metabolism and mood, specialists say the type and intensity of exercise matter.
Why Extreme Endurance Could Be A Problem
Doctors cautioned Lois against extreme endurance events such as half-marathons because prolonged, high-intensity training can significantly elevate cortisol, the body’s primary stress hormone.
In people with PCOS, hormonal balance is already fragile. Persistently high cortisol may:
- worsen insulin resistance
- disrupt ovulation further
- aggravate fatigue and inflammation
- intensify menstrual irregularities
In other words, although movement is beneficial, chronic physical stress can sometimes counteract the hormonal stability patients are trying to restore.
Moderate-intensity exercise, brisk walking, strength training and shorter runs, is generally considered more supportive for hormone regulation than sustained high-intensity endurance workloads.
From Half Marathon To Shorter Goals
Logan previously completed the London Landmarks Half-Marathon with Lois in 2024, describing the preparation as mentally and physically demanding. The pair had hoped to repeat the experience, but the new medical advice has changed those plans.
Instead, they now intend to focus on shorter runs together.
The television presenter admitted she felt a surprising sense of relief at the specialist’s recommendation, recalling how intense the training had been for both of them.
A sporting life continues — just differently
Lois, a competitive showjumper and university student, has long balanced academics with elite sport. She has ridden horses since childhood and competed at national levels, later even participating in a charity jockey race — an experience she described as “brutal.”
Her diagnosis does not end her athletic pursuits, but it reshapes them.
Medical experts increasingly stress that PCOS management is not about stopping exercise but tailoring it. Sustainable training, adequate recovery, and balanced nutrition often produce better long-term hormonal outcomes than relentless endurance performance.
For athletes with PCOS, the goal shifts from pushing physical limits to supporting physiological stability — a change that, doctors say, can ultimately protect both performance and health.
© 2024 Bennett, Coleman & Company Limited

