
Credits: Canva
Ignored, Misdiagnosed And At Risk: Why Women Need To Listen To Their Heart?
Even after decades of health education campaigns and medical breakthroughs, there is still one myth that dangerously persistent—the heart disease is a "man's disease." This misconception has contributed to a fatal blind spot in diagnosing, treating, and managing women across the globe. The reality is even more sinister: cardiovascular disease (CVD) is the world's biggest killer of women, killing more people annually than all cancers together.
What's even more troubling is that the problem continues to exist in the face of decades of data, research, and advocacy by groups such as the American Heart Association (AHA), who continue to raise the alarm. Women are being misdiagnosed, underdiagnosed, and undertreated—particularly young women and women of color—resulting in avoidable deaths and long-term health repercussions.
Young Women Are Facing More of Heart Disease
Once thought to be at risk only after menopause, young women are increasingly having heart attacks and other cardiovascular events. Increasingly, studies now indicate that heart disease is increasing among young women between the ages of 18 to 55, a trend that has puzzled experts and rendered emergency rooms unprepared to recognize early warning signs among this group.
These women aren't only falling ill to the disease—they're also more prone to be sicker and to fare worse than age-matched men. They face this with further delayed diagnoses, with research indicating that women wait an average of more than two days before describing heart attack symptoms, compared with 15 hours for men.
Some of the challenge is the way heart attacks manifest in women. Men usually see the hallmark symptom of crushing chest pain, but women tend to present with more insidious, unusual symptoms, such as:
- Shortness of breath
- Jaw, back, or neck pain
- Nausea or vomiting
- Indigestion
- A feeling of dread
- Unusual fatigue or palpitations
These symptoms are commonly misinterpreted—by both physicians and patients—into stress, anxiety, or gastrointestinal distress, resulting in delays in treatment. Indeed, women are less likely to be immediately provided an electrocardiogram (EKG) in the ER and frequently are released from the ER without proper diagnostics or treatment.
Why Women Are Misdiagnosed?
Apart from symptoms, the body physiology of a woman's heart is not the same as a man's, making things even more complicated. Women have smaller vessels, are more prone to microvascular disease, and have special types of heart attacks like spontaneous coronary artery dissection (SCAD) and myocardial infarction with nonobstructive coronary arteries (MINOCA). These are the kinds that don't register on standard tests, so women's heart attacks might be completely overlooked.
More disturbing is the inherent gender bias in healthcare. Studies indicate women and minorities spend more time in the ER waiting for treatment, are less likely to be hospitalized, and do not get prescribed life-saving medications following a heart attack. The AHA says 26% of women die within one year of experiencing their first heart attack, as opposed to 19% of men.
Pioneering cardiologists are dubbing it a global health crisis. A groundbreaking consensus statement by 33 specialists from the British Cardiovascular Society has provided a vision plan for closing these disparities. The statement is urging:
- Champions and specialist centers for women's heart health
- Equal diagnostics and treatments
- More women in clinical trials
- Care models that are culturally and gender-sensitive
It also draws attention to the fact that more than 3.6 million women in the UK alone suffer from ischemic heart disease, with most getting delayed or suboptimal treatment. This is replicated all over the world—from the US to South Asia—due to old-fashioned medical beliefs, societal prejudices, and ignorance.
What Women Can Do Right Now?
For far too long, women's voices—particularly when they are reporting pain or discomfort—have been ignored or trivialized. But your body remembers when something's amiss, and listening to your heart may save your life.
Here's what you can do:
Learn your risk factors—blood pressure, cholesterol, diabetes, and family history.
Speak up for yourself—question your doctor, ask for proper tests, and don't be afraid to seek a second opinion.
Pay attention to the signs—even if they don't fit the norm.
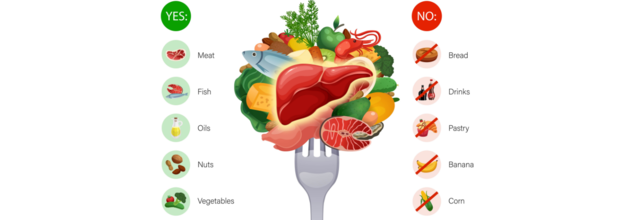
Live a heart-healthy life—eat healthfully, stay active, cope with stress, and have regular check-ups.
Women such as Stewart, a heart attack survivor and advocate for the AHA's Go Red for Women initiative, remind us that awareness alone is not sufficient. Education, action, and advocacy are needed to turn back the deadly tide of overlooked and undiagnosed heart disease in women.
Heart disease does not discriminate, yet the medical system still does. From delay in ER treatment to exclusion from clinical trials, women are perpetually an afterthought in the world of cardiovascular medicine. That has to end. Whether you are a 20-year-old woman, a mother managing stress, or a retired grandmother, your heart matters. And so does it deserve equal attention, equal care, and a more louder voice.

Credits: Canva
8 Reasons Why You May Have An Itchy Eye
People can have itchy eyes for various reasons. The reasons may include allergies, environmental pollutants, infection, and some conditions that can affect the eyes. The treatments could vary from home remedies to medical intervention.
Seasonal Allergies
If you have itchy eyes around the same time in the year, you may have seasonal allergies. You could be allergic to ragweed or something else that blooms during the season, releases pollen and gets into your eyes that time of the year.
You may also get reactions like sneezing and nasal congestion. Allergic symptoms are also triggered by histamine, which is a compound released by cells to defend against allergens. It causes an inflammatory response, and itchy eyes are one of the common signs of it.
So, what can you do?
- Pay attention to the local weather reports, look out for pollens.
- Keep your doors and windows locked.
- Take showers and wash clothes to keep pollen away.
- Wear a mask every time you stay outside.
To counter your allergies, you can also use over-the-counter astihismine medications, which can be helpful for controlling symptoms.
Perennial Allergies
They are not like seasonal allergies, they are the ones that stay year-long. Things like mold, dust, and pet dander could be the reason that can trigger perennial eye allergies.
You might be allergic to certain products around your home. Your contact lens solution could be bothering your eyes, or even your soap or shampoo might be the cause.
If you've already ruled out environmental allergens, try stopping the use of any product that comes into contact with your eyes. It may take some trial and error, but finding the source can make a big difference.
To know for sure if you have an allergy, an allergist can do a skin test. This involves putting small amounts of allergens—like ragweed or pet dander—just under your skin to check for a reaction. These tests are generally safe for both kids and adults.
Along with avoiding allergens, medications like antihistamines or corticosteroids can help reduce eye inflammation and discomfort.
Airborne Irritants
There could be people who are sensitive to smoke, diesel exhaust, or even certain perfumes. You could use soothing eye drops to cool the irritation.
Infection
Eye infections could come from viral, bacterial, and fungal infections. These all can make your eye itchy. One of the common infections is conjunctivitis, also known as pink eyes. It is very contagious and could be accompanied by drainage from the affected eye.
Other infections could be uveitis, which is an inflammation to the iris. Steroids may also help with this. The best way to deal with it is to see a doctor and get the right help.
Dry Eye
There could be a lot of reasons that can cause a dry eye. This happens when your tears dry out, which are made from combination of water, oil, and mucus to keep your eyes moist.
Diabetes could be the reason for dry eyes. Sometimes, a blocked tear duct or tear gland leads to dry and itchy eyes. Other reasons which may contribute to dry eyes are:
- antidepressants
- medications that lower blood pressure
- birth control pills
- decongestants
Eyestrain
If you look at your computer screens for a little too long, or try to read something in a poorly lit area, it can strain your eyes and they could feel very itchy and dry. In fact, driving for a long time, especially at night could also strain your eyes. It can also feel itchy, if it is too sunny.
Overusing Contact Lenses
Contact lenses also have to be used for a limited time period. If you have worn your contact lenses for too long, or have not replaced it, or washed them regularly, it can itch your eyes.
Blepharitis
Red and itchy eyes can sometimes be caused by blepharitis—an inflammation of the eyelids. This happens when the tiny oil glands near the base of your eyelashes get blocked. Keeping your eyelids clean can often help ease symptoms like swelling and watery eyes.
While blepharitis usually doesn’t affect your vision, it can become a long-term issue and may lead to conjunctivitis or other eye problems. In some cases, antibiotics or anti-inflammatory medicines may be needed to manage it and prevent complications.

Ozempic Face: Is The Weight Loss Drug Changing More Than Your Waistline?
Sunken faces, hollowed-out eyes, drooping jawlines—these aren't rumors; they're real physical changes seen in patients who experience quick fat loss due to the GLP-1 drug Ozempic and it's not just stopping at the face. The health world is now abuzz with terms like "Ozempic feet" and "Ozempic butt," showing the increasing fear that this hack to being thin could have unexpected physical trade-offs.
Ozempic, a drug initially designed for the treatment of type 2 diabetes, has recently swept the internet, not to treat the condition it was designed for, but with its remarkable off-label effects on weight reduction. Celebrities, social media influencers, and ordinary consumers are using this self-proclaimed "miracle injection" to lose weight quickly.
While the drug is all the rage on social media and among celebrities, experts are sounding alarms over its widespread, off-label usage. Are we settling for instant gratification rather than long-term health and aesthetics? Is Ozempic sneakingly reshaping not only bodies, but also the standards of beauty of an entire generation?
With new beauty trends spreading at lightning speed, a new buzzword taken the wellness world by storm- "Ozempic Face." With social media buzz and gossip about celebrities, the discussion of Ozempic, a type 2 diabetes drug turned off-label weight-loss phenomenon, has moved past glucose levels and waistlines—it's now transforming how we think about facial aging.
Celebrities such as Katy Perry, Lizzo, John Goodman, Karan Johar, Mindy Kaling, Ram Kapoor and even Oprah Winfrey have come under scrutiny for their facial changes reportedly tied to the Ozempic face phenomenon due to the noticeably changes in their faces.
Ozempic is the brand name for semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist produced by drug giant Novo Nordisk. Approved by the U.S. FDA in 2017 for the treatment of type 2 diabetes, it acts by mimicking the effect of GLP-1, a hormone that triggers insulin release, suppresses appetite, and decreases blood sugar.
Although its initial purpose was to regulate blood sugar in diabetic patients, Ozempic's appetite suppressant property gave rise to an unforeseen—though highly marketable—side effect: major weight loss. This off-label application has been widely adopted, particularly in Hollywood and high society, and it has become a first-choice treatment for those wanting quick, pharmacy-facilitated weight loss.
What is Ozempic Face?
While dramatic weight loss tales dominate the wellness feeds, another and more somber trend is being observed: "Ozempic Face." The latter is defined as facial side effects seen on some patients who undergo rapid fat loss, especially in the cheeks, temples, and jaw.
Common characteristics of Ozempic Face are:
- Sunken eyes and circles under the eyes
- Hollowed cheeks and temples
- Loose jowls and loose skin of the neck
- Enhanced prominence of fine lines and wrinkles
What makes this effect so dramatic is not only the transformation of body shape, but also the accelerated aging effect on the face, which can cause users to look gaunt or exhausted, even though their overall health indicators are getting better.
What Causes Ozempic Face?
While the name is catchy, Ozempic itself is not to blame—instead, it's the rate and amount of weight loss that leads to the facial alterations. The disappearance of subcutaneous fat from the face—fat that previously contributed volume and youthfulness—results in a more gaunt look. This is why it occurs:
Facial fat depletion: Fat loss is not confined. When you lose weight, you lose fat all over—yes, including the face.
Reduced skin elasticity: With age, the skin loses collagen and elasticity, making it harder to rebound after volume loss.
Rapid weight loss: When the transformation happens quickly, the skin doesn't have time to adjust, causing sagging and wrinkling.
It's also a side effect that appears in other GLP-1 medications or any rigorous calorie-cut weight reduction regimen. It's not unique to Ozempic—but the medication's growing popularity makes it a familiar case study.
Another strange side effect of the slimming drug is 'Ozempic feet' which is a described as\t the sloping, creased skin and hollow look of the feet especially at the top, where the skin naturally thins. This is a result of an extreme and rapid depletion of fat stores as the patients lose weight. Unlike intentional body sculpting or fat reduction from exercise, weight loss with Ozempic is fast and even, subjecting areas that typically have small fat reserves, such as the feet. Although weight loss is something to be cheered, the psychological cost of Ozempic Face is never talked about. Users say that they feel more self-conscious after they've reached their weight loss goal because of the unforeseen changes in their looks. In a society where youthfulness is highly valued, the side effects are extremely unsettling.
This has resulted in an increase in consultations with cosmetic surgeons and dermatologists, with the patients opting for fillers, tightening procedures for the skin, and even facelifts to counteract the effects of their prescription weight loss process.
Can You Prevent or Reverse Ozempic Face?
While it's impossible to prevent it completely, there are measures one can take to reverse the effects of Ozempic Face, especially if patients take a pro-active approach:
Gradually lose weight: Work closely with your doctor to adjust your dose and take a slower rate of weight loss.
Stay well-hydrated: Drink 1 to 2 liters of water per day to support skin health.
Make protein a priority: Eat a diet that includes lean meats, eggs, legumes, and fish to help support skin structure and elasticity.
Skincare regimen: Add collagen-stimulating and moisturizing products to your routine to enhance skin resilience.
Discuss aesthetic treatments: For more substantial changes, such as dermal fillers, radiofrequency tightening of the skin, and laser therapy, will restore lost volume and tighten lax skin.
Increased use of Ozempic off-label is challenging for healthcare practitioners. Although it can assist in weight control, extensive counseling is essential. The providers need to make sure the patients are informed about the potential physical and psychological effects—not simply the advantages.
In the meantime, those considering using semaglutide to slim down need to be told all about its body-wide effects, not just its effect on weight.
Ozempic craze has highlighted a deeper societal paradox- to become thin over the value we place on youthfulness. Although it may shrink waistlines, it does so at the risk of unintentionally aging the face—exposing the complex costs of modern standards of beauty.
World Liver Day 2025: What Extended Ketosis Really Does To Liver Enzymes And Function
For the millions of people globally, "healthy eating" is a privilege rather than a default choice. From high costs of healthy foods to nutritious food systems that favor profit over health, the obstacles to a liver-supportive diet are real. Among popular diets, the ketogenic diet, or keto, has become extremely popular for its fast weight loss advantages but beneath its high-fat, low-carb framework is a less-discussed issue—how prolonged ketosis can silently burden the liver.
Your liver is your body's control center for detoxification and metabolic regulation. It processes toxins, digests nutrients, produces bile to break down fats, stores energy, and even produces blood-clotting factors.
“While many factors shaping our diet lie outside personal control—like zoning laws, school meal policies, and labeling—what remains in our hands is the knowledge of how our food choices impact our health,” says Nutritionist and Diabetes & Inflammation Specialist, Khushboo Jain Tibrewala.
However, these processes can be easily undone by modern lives—too much booze, sweet diets, lazy lifestyles, and, ironically enough, some hardcore dietary regimes like prolonged keto. The liver's tough, true, but get it working around its metabolic tipping point for sustained periods, and it begins to exhibit symptoms—a lot of which come in the form of abnormal liver enzymes and inflammation.
What Is Ketosis?
Ketosis is a metabolic process by which your body shifts from glucose (carbohydrate) to fat fueling. Carbohydrates in your diet, under normal conditions, get digested into glucose, which gets utilized by the body as fuel. In ketosis, fats are metabolized into ketone bodies—an additional fuel for brain and muscle tissue.
As per Tibrewala, this condition can be triggered by, "A ketogenic diet—intentionally low in carbohydrates and high in fat, or in severe cases of uncontrolled diabetes, where glucose metabolism is disturbed."
Although created initially to control epilepsy, the keto diet is today mainstream. Individuals remain in ketosis for weeks, months, even years. But is such long-term adaptation liver-friendly?
Overburdening the Liver
"The liver is at the center of making ketones," Tibrewala says. "And that process of metabolism is taxing." Sustained levels of ketosis lead to the liver breaking down fats continuously, which in turn increases liver enzymes—namely ALT (alanine aminotransferase) and AST (aspartate aminotransferase).
Clinical research indicates that keto dieters who eat this way in the long term tend to develop signs of hepatic stress even when they do not have fatty liver disease. High enzymes don't necessarily mean instant damage to the liver—but they do signal that the liver is burning out. Left untreated, this can result in inflammation, fibrosis, or even non-alcoholic steatohepatitis (NASH) in vulnerable people.
Low-Carb, Low-Fibre
A significant downfall of ketosis is the drastic reduction of dietary fibre, a substance which is rich in carb-foods such as fruits, whole grains, and legumes. "Fibre is not only for digestion—it's food for your gut microbiome," adds Tibrewala.
A fiber-deficient diet upsets the balance of bacteria in the gut, permitting deleterious strains to dominate. The outcome? Increased permeability of the gut, systemic inflammation, and toxic load—altogether placing further stress on the liver. The organ is thus forced to struggle even harder to detoxify these toxins, added to its already high workload under ketosis.
Hidden Harm of Processed Keto Products
Ironically, most keto believers resort to processed foods to fulfill their macronutrient needs. From protein powders and MCT oils, snack bars, to exogenous ketone supplements, they are filled with preservatives, additives, and in some, heavy metals.
"These artificial substances are processed through the liver, which is yet another source of stress," Tibrewala observes. Gradually, this higher toxic load—combined with compromised gut integrity—can drive the liver toward pathology, even if there are no obvious symptoms.
Therapeutic vs. Trendy: When Does Ketosis Make Sense?
It’s important to acknowledge that ketosis, in short, supervised intervals, may have therapeutic potential—particularly for managing epilepsy, obesity, or insulin resistance. But long-term, unsupervised ketosis can be a slippery slope.
A liver in constant ketone-production mode is analogous to a machine running non-stop—it wears out faster. “Our liver thrives on balance, moderation, and nourishment—not on extremes,” emphasizes Tibrewala.
What Can You Do for Your Liver?
Select balanced nutrition: Eat whole grains, plant protein, and high fibre foods.
Steer clear of ultra-processed keto treats and go for whole-food fats such as avocado, nuts, and seeds.
Restrict ketosis to short cycles, if at all, and always after consulting a health professional.
Emphasize gut health with probiotics, prebiotics, and fermented foods. A healthy gut lightens the burden on your liver.
Drink water and move around—two simple but potent aids to liver detox and metabolic equilibrium.
In the quest for weight reduction or "biohacking," extended ketosis has been hailed as revolutionary but your liver- the powerhouse of your metabolism tends to take the hit.
Khushboo Jain Tibrewala is a Nutritionist and Diabetes & Inflammation specialist at The Health Pantry in India
© 2024 Bennett, Coleman & Company Limited

