
‘Fit and Healthy’ Woman Diagnosed With Terminal Colon Cancer- Her Symptoms Had Nothing To Do With The Gut
Colon cancer is commonaly linked to gastrointestinal problems—abdominal cramps, bloating, and stool blood. Not for 57-year-old Karen Kennerley, however, a special education teacher from Lancashire, England. None of these symptoms were experienced by her. All she felt was an abnormal and frequently downplayed symptom: tiredness.
Even though everyone around her considered her "fit and healthy," Karen's life was turned on its head when she received a stage 4 colon cancer diagnosis. The sole early warning sign? A sense of fatigue that drained her, one she had initially chalked up to the stress of her job. Today, as she receives treatment and battles for her life, her tale is a grim reminder to others regarding the silent threats of colon cancer.
Karen initially went to see her general practitioner (GP) in December 2022 because of ongoing fatigue. Being a hardworking teacher employed in a special educational needs (SEN) school, she felt that her tiredness was only due to extensive working hours. Her GP undertook standard blood tests, and these did not raise any initial alarm. Yet, as a precautionary measure, she was referred for a fecal immunochemical test (FIT) and a colonoscopy in January 2023.
In spite of assurances from doctors that she was healthy, Karen's colonoscopy showed a tumor in her large intestine. What was thought to be benign proved to be colon cancer, and she underwent extensive surgery in June 2023 to have the tumor and part of her intestine removed. She then had eight rounds of chemotherapy.
After her treatment, Karen anticipated returning to everyday life, convinced that she had won her struggle with cancer. Yet in March 2024, she was admitted to the hospital with suspected appendicitis. The truth was much more terrifying—her cancer had infected her ovaries, advancing to stage 4. She was told that the only treatment offered by the NHS was palliative chemotherapy, to prolong her life, not cure her.
"I was shattered, from being informed that I was benign, to being informed that I had stage three colon cancer, and then this," Karen explained. "There were just a lot of feelings—devastation, fear, disbelief."
Deciding to battle for her life, Karen sought out alternative therapies. She discovered Trans Arterial Chemoembolization (TACE), a focused cancer treatment in Germany. In contrast to conventional chemotherapy, TACE injects cancer-killing medications directly into the tumor, with the possibility of enhancing survival and minimizing side effects.
Karen had three cycles of TACE treatments, which cost £35,000 ($44,000 USD). Thankfully, her tumors started to reduce in size. Her finances were drained, however, and she is currently fundraising to pay for additional treatment.
"Treatment has been going well, but I need more of it. The stress and financial strain are overwhelming. I am unable to work, and my statutory sick pay will soon be gone," she said. "Stage 4 cancer patients feel abandoned. I wish to change this—not only for me, but for others battling this."
Importance of Early Detection in Colon Cancer
Karen's case brings to light an important problem: colon cancer usually comes with mild symptoms that may be ignored. Although frequent symptoms are:
- Blood in the stool
- Changes in bowel habits that persist
- Unintentional weight loss
- Abdominal discomfort or bloating
Fatigue is a lesser-known but important symptom. In Karen's case, this initial symptom was first explained away as typical work-related fatigue. But it proved to be a sign of a serious underlying illness.
Medical professionals emphasize the need for regular screenings, particularly for people over 45, or earlier if there is a family history of colon cancer. A FIT test, which identifies occult blood in stool samples, is a quick and useful screening test.
Karen's situation is not rare. Colon cancer is the third most frequent cancer globally, both in men and women. The World Health Organization (WHO) states that early detection is essential in enhancing survival. Despite this, patients are often diagnosed at advanced stages because of imprecise or ignored symptoms.
Younger adults have also experienced an increase in colorectal cancer cases in recent years, leading researchers to explore possible causes like diet, lifestyle, and genetics. Public awareness campaigns stress the importance of identifying even non-digestive symptoms, including fatigue, anemia, and unexplained weakness.
Aside from her own struggle, Karen wishes to speak out on behalf of improved support mechanisms for stage 4 cancer patients. Most people in her situation feel abandoned by healthcare systems that prioritize curative treatments for early-stage cancers, leaving those with advanced diagnoses with few options.
"I don't want to fight for myself alone—I want to fight for all those who are going through stage 4 cancer. We deserve better than to be told to get ready for the end," she exclaimed.
Karen continues to fundraise to keep up with treatment and raise awareness about listening to your body. "I want people to realize that you don't need to have dramatic symptoms for it to be cancer. If something doesn't feel right, don't ignore it—get checked."
Karen Kennerley's case serves as a testament to how cancer may manifest in unexplained manner. She is struggling for survival even as she is fighting to get awareness raised on cancer by appealing to others to place priority on their own health and going for a doctor even at slightest deviations from health.

Credits: Canva
Why More Women Are Choosing To Have Kids In Their 30s Even As Fertility Drops?
For decades, the ideal age for women to become mothers was firmly rooted in the 20s—a peak period conventionally tied to prime fertility, social norms, and the onset of family life. However, recent information reveals a different picture, more women are increasingly opting to start families when they are in their 30s, although fertility does start decreasing with age. Based on initial data from the Centers for Disease Control and Prevention (CDC), women aged 30 to 34 now have more births than women in their late 20s, a big cultural and demographic change.
This article explores into what's behind this shift—from changing social values and economic considerations to medical innovations and individual empowerment.
In 2016, the CDC also said that the birth rate for women between the ages of 30 and 34 was 103 per 100,000, just barely above the 102 per 100,000 for women between the ages of 25 and 29. The mean age at which American women are giving birth to their first child has also increased to 28, from 26 only a few years earlier. This change signals something more than mere preference; it indicates greater systemic shifts within education, relations, and economic scenarios.
Women aged in their late 20s had the country's peak birth rates for over three decades. That storyline is being revised now. Authorities are attributing the change to a range of interrelated reasons—the primary among them being a decision to wait until marriage to come later in favor of a career or self-realization phase first.
Is Rise of Professional and Financial Independence the Reason?
Women of the millennial and Gen Z generations are entering a job market where education and career mobility are prized—and in many cases, a necessity for financial security. With women becoming more prevalent in positions of leadership within industries and with record-breaking levels of educational attainment, motherhood is no longer viewed as a duty of youth but as a thoughtful life choice.
Waiting until later to have a child offers the time necessary to acquire financial stability, establish a robust professional base, and even eliminate student loans. These actions are important in an environment where living costs and child-rearing—particularly in metropolitan areas—keep increasing.
Deeply connected to this movement is the shifting attitude toward marriage. The first marriage age in America has climbed to 27 for women, a drastic increase over earlier generations. As people delay marriage or pursue alternative relationship structures, the timing of having children has naturally followed suit.
Relationship expert Bill Albert of the National Campaign to Prevent Teen and Unplanned Pregnancy observes that cultural trends, such as the continued decline in teen pregnancies, are part of a larger movement toward thoughtful parenting—where a person is prepared emotionally and economically before assuming the responsibility of bringing a child into the world.
Fertility, Egg Freezing, and Reproductive Health Awareness
Although the social clock might be ticking later, biology hasn't. A healthy woman has approximately a 20% chance of conceiving in any menstrual cycle in her 20s, says the American Congress of Obstetricians and Gynecologists. Fertility, however, starts to decline in the early 30s and declines more steeply after age 37.
Despite this, women are becoming more attuned to these biological facts—and are doing something about it. Egg freezing is becoming a proactive solution, enabling women to freeze their eggs as they work toward other objectives in life. Even though the treatment is expensive (usually more than $10,000, with yearly storage charges), its popularity speaks volumes for the contemporary woman's willingness to seize control of her reproductive destiny.
Infertility Support and Treatment Options
To those who do experience fertility issues, advances in medicine have made family creation more possible than ever. The CDC reports that approximately 11% of women aged 15 to 44 have utilized infertility services, and the Mayo Clinic explains several causes—ranging from ovulation problems and PCOS to endometriosis and cancer treatment complications.
For couples seeking to become pregnant, lifestyle issues such as smoking, weight imbalance, and stress can be factors as well. Health professionals advise women older than 35 to have an evaluation after six months of failing to conceive—six months less than for younger women. With various treatments such as IVF, hormone therapy, and assisted reproductive technologies, increasing numbers of women in their 30s are having successful pregnancies despite the loss of function that comes with age.
Emotional Readiness and the Psychology of Modern Motherhood
Aside from biology and economics, there's the issue of emotional readiness. Women say they feel more grounded, self-assured, and self-aware in their 30s. They've had time to travel, learn, experience the world, and develop a strong sense of self prior to embracing the challenging and life-altering role of motherhood.
This emotional maturity will also feed through into more secure parenting arrangements and more settled family lives. More mature age at motherhood will also include women who have long-term partnership experience and securely structured support networks behind them.
The motherhood narrative is shifting. Women today are rewriting the playbook, using fertility with deliberation and knowledge, and turning conventional wisdom on its head when it comes to the "right" time to have children. While age still plays a huge role in reproductive health, it is no longer the sole factor.
As the world continues to evolve—socially, economically, scientifically, it's bound to happen more and more often that women continue to look on their 30s not as a deadline but as an opening. And as they gain ever-improved access to fertility procedures, as wider society offers their support, as medicine makes breakthrough after breakthrough, they'll have more control over motherhood than ever before to enter into when they want.
Credits: Northwestern Medicine
Breathlessness During Pregnancy? Cough Turned Out To Be Stage 3 Melanoma For This Woman; Doctors Share Details
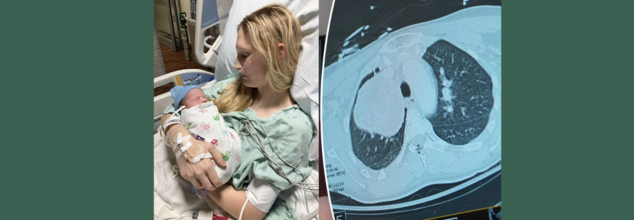
What started out as a persistent cough while pregnant almost turned into a tragedy for 26-year-old Illinois' MaKenna Lauterbach. At 36 weeks' pregnancy, the would-be mom thought that her symptoms were normal for pregnancy exhaustion in late stages—until she started gasping for air from doing minor chores. What ensued was a time-sensitive, life-saving battle of wits between world-class experts, state-of-the-art medical treatments, and an outcome against all odds.
Pregnancy tends to be accompanied by fatigue, shortness of breath, and changing physical needs. So when MaKenna began feeling breathless and having a persistent cough while caring for her horses, she attributed it to third-trimester exertion. Walking to the barn made her breathless—as if she'd run a marathon. But her symptoms did not get better, and by the time she was full term, her condition had progressed dramatically.
Even with her deteriorating symptoms, imaging tests were initially shunned. Medical staff are naturally averse to putting pregnant women through the stress of radiation exposure, particularly when in the late stages of pregnancy. But MaKenna's condition rapidly worsened—coughing gave way to vomiting and intense respiratory distress, prompting emergency admission to hospital.
Just a few days from her due date, imaging at last showed the devastating discovery—a grapefruit-sized tumor wedged in her chest, obstructing the artery to her right lung. The tumor was suffocating her airway and threateningly restricting oxygen delivery, placing mother and baby alike in danger.
MaKenna was flown to Northwestern Memorial Hospital in Chicago, where she was admitted to the intensive care unit. Within a short time after arrival, she went into labor. Her blood pressure rose, the baby became distressed, and physicians realized that they had only hours—possibly minutes—to move.
"Her lungs were impaired because of the tumor, and labor was also slowing her down to breathe. The danger of respiratory failure and cardiac arrest was very real," said Dr. Lynn Yee, a maternal-fetal medicine specialist at Northwestern Medicine.
MaKenna was put on extracorporeal life support (ECMO)—a life-supporting device that circulates oxygenated blood outside of the body—and received an emergency C-section. Her baby boy, Colter, was delivered safely, healthy in spite of the wild ride he had getting here.
For MaKenna, there was a mix of joy and fear. "Because of the tumor, the delivery came so rapidly. I was mourning the birth plan I had been planning for months, while also coping with the news of my surprise diagnosis," she explained.
What is Rare and Aggressive Melanoma?
After the birth, physicians initiated additional tests. A bronchoscopy test showed the tumor was stage 3 melanoma—a skin cancer that had somehow traveled and developed inside her chest.
This posed a singular challenge. "There isn't much written about or a lot of published cases on how to treat melanoma that comes in this way," said Dr. Kalvin Lung, a thoracic surgeon at Northwestern Medicine. "We had to fall back on the knowledge our team has gained from years of taking care of complex thoracic cases."
Prior to surgery, doctors gave three doses of immunotherapy to shrink the tumor. The therapy was effective in diminishing its size from 13 centimeters to 9 centimeters, thus enabling the subsequent action—surgery.
The procedure itself was extremely complicated. Dr. Lung and Dr. Chris Mehta, a cardiac surgeon with Northwestern Medicine, were required to remove MaKenna's right lung entirely, part of the pulmonary artery, and related lymph nodes. The tumor had invaded large blood vessels and spread throughout all three lobes of the right lung. "We may have a case like this every few years," said Dr. Mehta.
Now 27, MaKenna is stable and continues her immunotherapy treatments. Her scans show no new signs of metastatic cancer, and the tumor site remains inactive. She’s focusing on motherhood, recovery, and gratitude.
“Colter is the best baby—always smiling and sleeping through the night,” she said. “I can’t say enough about the incredible medical team that saved my life. Because of them, I’m here today.”
Dr. Yee continued, "To see MaKenna doing so well, and Colter thriving, brings tears to my eyes. It demonstrates what coordinated, compassionate medical care can do."
Can Pregnancy Shadow Life-Threatening Illnesses?
Pregnancy is commonly accompanied by a variety of physical changes—fatigue, shortness of breath, backaches, nausea, and swelling. Although these symptoms are typically harmless, they sometimes mask the signs of serious underlying medical conditions. This crossover between normal pregnancy pains and signs of potentially fatal diseases can mean that the illnesses are not diagnosed until late, as in the recent case of MaKenna Lauterbach—a 26-year-old woman whose relentless cough and shortness of breath throughout her pregnancy proved to be stage 3 melanoma in her chest.
Shared Symptoms of Pregnancy and Illness Mimic One Another
Most life-threatening conditions have symptoms that are identical to those of pregnancy. Diseases such as heart disease, blood clots, infections, and even cancer may appear with fatigue, chest pain, shortness of breath, or swelling—commonly attributed to normal pregnancy complaints. This similarity results in a diagnostic blind spot.
For example:
- Shortness of breath can be due to increased oxygen demand during pregnancy but can also result from lung disease or heart failure.
- Swelling in late pregnancy is normal but may indicate preeclampsia, kidney disease, or a tumor compressing veins.
- Nausea and vomiting are usual in the first trimester but may also obscure gastrointestinal cancers or liver disease.
Hesitation With Diagnostic Imaging in Pregnancy
One of the greatest difficulties is that physicians tend to shun some diagnostic tests such as X-rays, CT scans, or MRIs during pregnancy in order to avoid exposing the fetus to radiation. Although this prudence is necessary, it can lead to life-threatening delays if a critical condition is suspected but not diagnosed. In MaKenna's situation, imaging was delayed until her symptoms became critical—by that time, a tumor had obstructed large lung arteries.
Immune and Hormonal Alterations Can Speed Up Underlying Disorders
Pregnancy dampens some immune reactions to shield the developing fetus. Yet, this changed immune environment can give rise to or speed up latent diseases like cancer, autoimmune disorders, or infections. Hormonal spikes can also nourish hormone-sensitive tumors, elevating the risk of complications.
Fetal Over Maternal Prioritization in Emergency Situations
During emergencies, choices are frequently made to safeguard the baby—even at the expense of delaying the mother's treatment. This preference can make cases more complex when the mother's declining health impacts fetal welfare directly. Delayed diagnosis or treatment of maternal illness can put both lives at increased risk.
Emotional and Cognitive Biases
Numerous pregnant women—such as MaKenna—will minimize their symptoms, assuming they are just a result of pregnancy demands. There is also a cultural pressure to suffer through pregnancy, and this can cause women not to speak up or seek second opinions when something does not feel right.
Pregnant patients with severe medical issues frequently need treatment from several specialists: obstetricians, oncologists, cardiologists, or pulmonologists. Without an integrated and coordinated effort, important warning signs can be overlooked or insufficiently explored. MaKenna's survival was partly because of the rapid collaboration between maternal-fetal medicine, thoracic surgery, oncology, and intensive care specialists.
Pregnancy never needs to stand in the way of diagnosing and treating potentially life-threatening diseases. Awareness, early investigation, and multidisciplinary care are critical in distinguishing normal pregnancy symptoms from red flags. Pregnant women must always feel confident enough to voice their concerns, clarify the situation, and stand up for their well-being—because, as MaKenna's experience demonstrates, an early diagnosis can save not just one, but two lives.

Credits: Canva
How Electrical Stimulation Is Quietly Transforming Psychiatry
Over the past two decades, a lot has changed in psychiatry. The field has embraced many unexpected tools, including electricity. Once largely the realm of pharmaceuticals and talk therapy, the field is undergoing a technological evolution powered by devices that target the brain's circuitry. This is known as electroceuticals. These approaches offer new hope for people with severe, treatment-resistant psychiatric disorders such as depression and obsessive-compulsive disorder (OCD).
The Rise of Electroceuticals
These usually refer to therapies that use electrical stimulation to modulate nervous system activity. These technologies aim to correct misfiring circuits in the brain, much like how a pacemaker regulates the heart. The therapies now being studied or offered include:
- Deep Brain Stimulation (DBS)
- Vagus Nerve Stimulation (VNS)
- Transcranial Magnetic Stimulation (TMS)
- Focused Ultrasound Neuromodulation
While many of these interventions are still being evaluated for efficacy in psychiatric care, they are already in use for neurological conditions like Parkinson's disease. It lend credibility to the crossover.
Chemical Imbalance And Beyond
Historically, psychiatry has operated on the assumption that mental illnesses stem primarily from chemical imbalances. This led to a focus on medications like SRRIs. However, recent research began shifting the focus from brain chemistry to brain circuitry. Neurosurgeons and psychiatrists alike now see disorders like depression not as chemical shortages but as network dysfunctions - where certain brain circuits fall to properly connect or regulate mood and behavior.
The shift is also shown in the treatment of major depressive disorder (MDD) with DBS. Electrodes implanted deep in the brain deliver high-frequency pulses to specific regions believed to be involved in mood regulation. Though still considered experimental for depression by the US Food and Drug Administration (FDA), DBS is FDA-approved for treatment-resistant OCD and shows promise in clinical trials.
Treatment-Resistant Disorder - Searching For The Solution
As per reports, an estimated 30% of people with depression and up to 60% with OCD do not respond to traditional treatments. For these individuals, electroceutical may also represent the only available hope. The access, however, is still very limited. The reason is cost and insurance coverage. However, with devices like VNS and TMS, which have now gained FDA clearance and some insurance support, the accessibility has been better. Though DBS and focused ultrasound remain largely available only through clinical trials.
The emotional and physical toll on patients can be considerable. Surgeries carry risks—such as infection, hemorrhage, or hardware complications—and require significant recovery time. Even successful cases often need supplementary treatments like medication or psychotherapy to sustain benefits.
What Technologies Are Available?
Deep Brain Stimulation (DBS): Involves implanting electrodes in the brain to stimulate key regions. It has shown success in regulating mood in patients with severe depression and OCD. Some report life-changing relief after decades of suffering, although results vary.
Vagus Nerve Stimulation (VNS): Sends signals via the vagus nerve to influence brain activity. Approved for treatment-resistant depression, its effectiveness is debated, with mixed outcomes in clinical trials.
Transcranial Magnetic Stimulation (TMS): Uses magnetic pulses delivered through a coil placed on the scalp. It’s non-invasive and increasingly accessible, though it requires multiple sessions and benefits may fade over time.
Focused Ultrasound: The newest contender, it uses sound waves to either ablate or modulate deep brain tissue. Still in early research stages, it’s entirely non-invasive and could become a game-changer due to its precision and safety profile.
© 2024 Bennett, Coleman & Company Limited

