
Image Credit: Canva
This Simple Eye Test Could Save You From Stroke, New Study Suggests
The human eye has long been considered a window to the soul, but modern science reveals its potential for being a diagnostic window toward our health. Researchers have already discovered that in the retina – the light-sensitive layer at the back of the human eye – resides an intricate network of blood vessels that can foretell crucial elements about a person's risk to stroke. This finding is a non-invasive and accessible approach to predicting stroke, hence challenging the dependency on the classic risk factors alone, such as high cholesterol or blood pressure. Recent research published in the journal Heart identified a "vascular fingerprint" in the retina, comprising 29 indicators of blood vessel health.
This fingerprint can predict the likelihood of a stroke with accuracy comparable to conventional methods. These indicators include characteristics like the density, twistedness, and complexity of retinal veins and arteries, which mirror the vascular architecture of the brain.
This innovative approach is particularly promising for primary healthcare settings and resource-constrained environments, where invasive lab tests may not be feasible. The potential to assess stroke risk through a simple retinal scan marks a significant leap in preventive medicine.
The researchers, who include those from The Royal Victorian Eye and Ear Hospital in Australia, analyzed fundus images, which are specialized photographs of the retina from more than 68,000 participants in the UK Biobank dataset. Over an average follow-up period of 12.5 years, 749 of those participants had a stroke.
The researchers used advanced machine learning models, such as the Retina-based Microvascular Health Assessment System (RMHAS), to study 30 indicators in five key categories of retinal vascular architecture.
These categories included calibre, which measured the length, diameter, and ratio of veins and arteries; density, which focused on the distribution of blood vessels in the retina; twistedness, analyzing the curvature and patterns of the vascular network; branching angle, which examined how veins and arteries split into smaller branches; and complexity, which evaluated the overall intricacy of the vascular network. In the study, age, sex, socioeconomic status, lifestyle habits, and health parameters, including blood pressure and cholesterol levels, were taken into account to ensure that the findings were robust. The analysis showed that 29 out of 118 retinal vascular indicators are significantly associated with first-time stroke risk.
Changes in density indicators corresponded to 10-19% increased risks of stroke; alterations in calibre indicators were accompanied by a 10-14% increase. Other studies have suggested that decreases in complexity and twistedness indicators corresponded to a 10.5-19.5% higher risk of stroke. These data support the retinal imaging non-invasive diagnostic tool for prediction of early stroke.
Amazingly, the retinal vascular fingerprint alone, in combination with only age and sex, was as good at predicting stroke risk as traditional methods that rely on invasive tests.
How the Retina is Connected to your Brain
Retinal blood vessels bear anatomical and physiological resemblance to those in the brain. Given this, it is an attractive organ for understanding the systemic health of the vasculature. Many diseases, for example, which damage blood vessels throughout the body, leave evidence in the retinal microvascular network. Diabetic retinopathy and hypertensive retinopathy are examples.
The study does have several limitations with this being an observational research, and so it cannot claim to establish any cause-and-effect relationships. The research was also primarily conducted on whites, which makes the findings a little less generalizable to a diverse population. Future studies would be better in including a range of ethnicities and exploring the risk of stroke associated with the type of stroke.
Simple Method To Detect Stroke Risk
Traditional stroke risk assessment is often confined to blood studies and imaging studies; however, these tools are not freely available in some low-resource settings. Retinal photography provides a completely non-invasive imaging modality. All that will be needed will be a basic photograph of an eye.
It is, therefore, through the introduction of artificial intelligence that has been a game-changer in retinal imaging. Systems like RMHAS rely on machine learning to pick out patterns and biomarkers that the human eye might not identify. Such improvements not only enhance predictive accuracy but also speed up the process while making it more cost-effective.
Also Read: 3 Shocking Stroke Risk Factors You Need To Control NOW
Prevention of Stroke through Early Detection
Stroke is one of the leading global health concerns, causing nearly 100 million cases a year and killing 6.7 million people. The majority of the cases are due to modifiable risk factors, including high blood pressure, poor diet, and smoking. The early warning system could help individuals and healthcare providers act proactively on these risks by providing an early warning system.
The discovery of the vascular fingerprint of the retina as a predictor of stroke risk is a testament to the power of innovative diagnostics. This non-invasive, accessible method may revolutionize stroke prevention, especially in underserved communities. As research continues to refine this approach and broaden its applicability, the eye may soon become an essential tool in safeguarding our brain health.
Every Day Tips to Prevent Stroke and Detect Risks Early
The good news is that strokes can be prevented in most cases by living a healthy lifestyle, coupled with knowing the early warning indicators. Implement these tips daily and prevent your risk for stroke before it gets too late.
- High blood pressure is one of the leading risk factors for stroke. Uncontrolled hypertension can weaken blood vessels, making them more prone to rupture or blockage. Invest in a home blood pressure monitor to check your readings regularly. Maintain a target of 120/80 mmHg by reducing salt intake, staying physically active, and adhering to prescribed medications.
- Unhealthy eating habits, such as diets with high levels of processed foods, saturated fats, and cholesterol, can lead to obesity and blocked arteries. A diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats is key. Include leafy greens, berries, nuts, and fish high in omega-3s, which help maintain cardiovascular health.
- Regular physical activity lowers the risk of high blood pressure, obesity, and diabetes, three leading causes of stroke. Try to engage in at least 150 minutes of moderate-intensity aerobic activity a week. Examples include brisk walking, cycling, or swimming. Also incorporate strength training to help strengthen your blood vessels.
- Smoking harms your blood vessels, promotes blood clots, and reduces the oxygen in your blood. Overconsumption of alcohol can raise your blood pressure and lead to weight gain. Quit smoking with support groups, counseling, or nicotine replacement therapy. Limit your intake of alcohol to moderate levels; that is, one drink a day for women and two for men.
- Unmanaged conditions, such as diabetes, high cholesterol, and atrial fibrillation, significantly increase stroke risk. Work with your healthcare provider to monitor and manage these conditions. For example, maintain blood sugar levels within target ranges for diabetes and take anticoagulants if diagnosed with atrial fibrillation.
- Obesity strains the cardiovascular system and increases the risk for stroke. Have a healthy diet along with regular exercise to have a sustainable weight loss. Small, consistent changes in, say, portion control or simply not having too many sugary drinks may make a big difference.
- As a result of this, dehydration could thicken blood, then clots might form. Drink at least 8-10 glasses of water per day. Include hydrating foods like cucumbers and watermelon in your diet, especially during hot weather or exercise.
- Poor sleep quality increases blood pressure, triggers inflammation, and raises stroke risk. Ensure 7-8 hours of sleep at night. Develop a bedtime routine: reduce screen time, have a regular schedule, and avoid caffeine close to bedtime.
- Acting fast during a stroke can prevent long-term damage and save lives. Learn the FAST acronym:
F: Face drooping
A: Arm weakness
S: Difficulty speaking T: Time to call 911
- Regular medical check-ups can identify and manage stroke risk factors before they lead to a stroke. Make an annual physical to track cholesterol, blood pressure, and other essential health markers. If you have a family history of stroke, discuss retinal imaging or carotid artery screening with your physician.
Retinal vascular fingerprints predict incident stroke: findings from the UK Biobank cohort study. Heart. 2025

Credits: UNICEF
Polio Cases On The Rise Again, WHO Warns The World To A Growing Threat
The international public health community was hopeful that polio—the crippling viral illness that previously paralyzed hundreds of thousands of children every year—was almost extinct. But in a concerning twist in 2025, the World Health Organization (WHO) has raised the alarm- polio is back, and eradication hangs in the balance.
In 2020, the world celebrated a milestone—polio was officially eradicated everywhere except two nations. But in the first quarter of 2025, an old nemesis has reappeared. Cases of wild poliovirus are again increasing in Pakistan and Afghanistan, the final two bastions of endemic transmission. Pakistan, which had reported 74 cases in 2024, has already seen 6 new cases this year. Afghanistan is not far behind with 1 reported case.
While the numbers are small in themselves, they portend a worrisome trend in a decades-long fight. Global health professionals point to interruptions of vaccine campaigns—interruptions they say are directly caused by deep reductions in international assistance.
One major factor behind this upsurge is the abrupt interruption of funding support from the United States Agency for International Development (USAID). USAID has long been a pillar of support for vaccination activities in polio-endemic and high-risk areas by financing personnel, logistics, vaccine sourcing, and outreach.
A private memo by Nicholas Enrich, USAID acting assistant administrator for global health, cautions that if these pauses in funding continue, we will witness another 200,000 cases of polio paralysis each year, and hundreds of millions more are at risk of being infected. The International Rescue Committee (IRC), which was carrying out polio vaccinations under the watch of the Ministry of Health and World Vision in Kenya, says its USAID-funded program was the initial one to close on January 31st.
"Right now, IRC support for polio immunization in Kenya's hard-to-reach areas has come to a halt," confirms Mohamed El Montassir Hussein, Kenya's IRC country director. Although local health officials are still immunizing, their efforts are strained without foreign funding.
Why Does Wild Polio Persist in Just Two Countries?
Pakistan and Afghanistan are the exceptions to an otherwise polio-free world. Several chronic challenges, according to experts, include unstable security environments, misinformation, religious and political opposition to vaccination, and weak health infrastructures. Additionally, vaccination teams working in war zones frequently encounter logistical challenges and safety threats.
The virus has been extremely resilient. It takes advantage of holes in immunity caused by lack of vaccinations. Adding to the problem is the presence of circulating vaccine-derived poliovirus (cVDPV)—an uncommon event whereby the attenuated virus contained within oral polio vaccines changes and becomes virulent again.
WHO Flags High-Risk Nations and Rising Global Concern
The WHO has listed five countries with the immediate risk of the international spread of polio:
- Afghanistan
- Pakistan
- Mozambique
- Democratic Republic of Congo
- Guinea
Furthermore, 35 nations have recorded imported cases of cVDPV type 2, while 10 countries continue to experience active circulation of wild-type or vaccine-derived poliovirus in the last 24 months. WHO's guidelines are:
- Improved vaccine coverage
- Increased access to healthcare in risk areas
- Travel restrictions for unvaccinated travelers from high-risk areas
But with more than $200 million in donor funding lost— including life-saving funds from the U.S. President's Emergency Plan for AIDS Relief (PEPFAR)—these guidelines encounter tremendous implementation challenges.
Hidden Cost of Underfunding Global Health
It is the invisible spread that makes the situation more threatening. Those countries with weak surveillance systems may not see early outbreaks until it becomes too late. In politically unstable or humanitarian crisis-affected areas, the virus can spread quietly among unvaccinated groups, only to spill over borders.
Polio flourishes in these crevices—between the unvaccinated, the untracked, and the neglected. And once it establishes itself, retaking control is that much harder and costly.
Although the numbers as they stand are alarming, they also create an opportunity for recommitment on a global scale. Global polio eradication has always been a collective endeavor. Today, more than ever, a concerted effort is needed.
WHO Director-General Dr. Tedros Adhanom Ghebreyesus reacted with strong concern over the diminishing U.S. support and asserted the urgency for international collaboration. "The precipitous cuts to U.S. funding also affect efforts to stop polio for good," he cautioned.
Relaunching public confidence in vaccines, maintaining secure access during times of conflict, reinstating funds channels, and reinforcing surveillance form part of the arsenal necessary to complete the mission against polio.
The resurgence of polio in 2025 is a wake-up call. It reminds the world that public health victories, no matter how close, can unravel quickly without consistent investment and collaboration.
Eradiating polio was never a matter of one country or one continent. It was about a shared global commitment. If the trend continues, we will risk wasting decades of progress—and allowing a preventable disease to reassert its hold on the world's most vulnerable.

Credits: Canva
Why More Women Are Choosing To Have Kids In Their 30s Even As Fertility Drops?
For decades, the ideal age for women to become mothers was firmly rooted in the 20s—a peak period conventionally tied to prime fertility, social norms, and the onset of family life. However, recent information reveals a different picture, more women are increasingly opting to start families when they are in their 30s, although fertility does start decreasing with age. Based on initial data from the Centers for Disease Control and Prevention (CDC), women aged 30 to 34 now have more births than women in their late 20s, a big cultural and demographic change.
This article explores into what's behind this shift—from changing social values and economic considerations to medical innovations and individual empowerment.
In 2016, the CDC also said that the birth rate for women between the ages of 30 and 34 was 103 per 100,000, just barely above the 102 per 100,000 for women between the ages of 25 and 29. The mean age at which American women are giving birth to their first child has also increased to 28, from 26 only a few years earlier. This change signals something more than mere preference; it indicates greater systemic shifts within education, relations, and economic scenarios.
Women aged in their late 20s had the country's peak birth rates for over three decades. That storyline is being revised now. Authorities are attributing the change to a range of interrelated reasons—the primary among them being a decision to wait until marriage to come later in favor of a career or self-realization phase first.
Is Rise of Professional and Financial Independence the Reason?
Women of the millennial and Gen Z generations are entering a job market where education and career mobility are prized—and in many cases, a necessity for financial security. With women becoming more prevalent in positions of leadership within industries and with record-breaking levels of educational attainment, motherhood is no longer viewed as a duty of youth but as a thoughtful life choice.
Waiting until later to have a child offers the time necessary to acquire financial stability, establish a robust professional base, and even eliminate student loans. These actions are important in an environment where living costs and child-rearing—particularly in metropolitan areas—keep increasing.
Deeply connected to this movement is the shifting attitude toward marriage. The first marriage age in America has climbed to 27 for women, a drastic increase over earlier generations. As people delay marriage or pursue alternative relationship structures, the timing of having children has naturally followed suit.
Relationship expert Bill Albert of the National Campaign to Prevent Teen and Unplanned Pregnancy observes that cultural trends, such as the continued decline in teen pregnancies, are part of a larger movement toward thoughtful parenting—where a person is prepared emotionally and economically before assuming the responsibility of bringing a child into the world.
Fertility, Egg Freezing, and Reproductive Health Awareness
Although the social clock might be ticking later, biology hasn't. A healthy woman has approximately a 20% chance of conceiving in any menstrual cycle in her 20s, says the American Congress of Obstetricians and Gynecologists. Fertility, however, starts to decline in the early 30s and declines more steeply after age 37.
Despite this, women are becoming more attuned to these biological facts—and are doing something about it. Egg freezing is becoming a proactive solution, enabling women to freeze their eggs as they work toward other objectives in life. Even though the treatment is expensive (usually more than $10,000, with yearly storage charges), its popularity speaks volumes for the contemporary woman's willingness to seize control of her reproductive destiny.
Infertility Support and Treatment Options
To those who do experience fertility issues, advances in medicine have made family creation more possible than ever. The CDC reports that approximately 11% of women aged 15 to 44 have utilized infertility services, and the Mayo Clinic explains several causes—ranging from ovulation problems and PCOS to endometriosis and cancer treatment complications.
For couples seeking to become pregnant, lifestyle issues such as smoking, weight imbalance, and stress can be factors as well. Health professionals advise women older than 35 to have an evaluation after six months of failing to conceive—six months less than for younger women. With various treatments such as IVF, hormone therapy, and assisted reproductive technologies, increasing numbers of women in their 30s are having successful pregnancies despite the loss of function that comes with age.
Emotional Readiness and the Psychology of Modern Motherhood
Aside from biology and economics, there's the issue of emotional readiness. Women say they feel more grounded, self-assured, and self-aware in their 30s. They've had time to travel, learn, experience the world, and develop a strong sense of self prior to embracing the challenging and life-altering role of motherhood.
This emotional maturity will also feed through into more secure parenting arrangements and more settled family lives. More mature age at motherhood will also include women who have long-term partnership experience and securely structured support networks behind them.
The motherhood narrative is shifting. Women today are rewriting the playbook, using fertility with deliberation and knowledge, and turning conventional wisdom on its head when it comes to the "right" time to have children. While age still plays a huge role in reproductive health, it is no longer the sole factor.
As the world continues to evolve—socially, economically, scientifically, it's bound to happen more and more often that women continue to look on their 30s not as a deadline but as an opening. And as they gain ever-improved access to fertility procedures, as wider society offers their support, as medicine makes breakthrough after breakthrough, they'll have more control over motherhood than ever before to enter into when they want.
Credits: Northwestern Medicine
Breathlessness During Pregnancy? Cough Turned Out To Be Stage 3 Melanoma For This Woman; Doctors Share Details
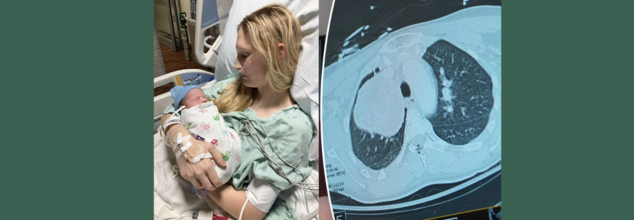
What started out as a persistent cough while pregnant almost turned into a tragedy for 26-year-old Illinois' MaKenna Lauterbach. At 36 weeks' pregnancy, the would-be mom thought that her symptoms were normal for pregnancy exhaustion in late stages—until she started gasping for air from doing minor chores. What ensued was a time-sensitive, life-saving battle of wits between world-class experts, state-of-the-art medical treatments, and an outcome against all odds.
Pregnancy tends to be accompanied by fatigue, shortness of breath, and changing physical needs. So when MaKenna began feeling breathless and having a persistent cough while caring for her horses, she attributed it to third-trimester exertion. Walking to the barn made her breathless—as if she'd run a marathon. But her symptoms did not get better, and by the time she was full term, her condition had progressed dramatically.
Even with her deteriorating symptoms, imaging tests were initially shunned. Medical staff are naturally averse to putting pregnant women through the stress of radiation exposure, particularly when in the late stages of pregnancy. But MaKenna's condition rapidly worsened—coughing gave way to vomiting and intense respiratory distress, prompting emergency admission to hospital.
Just a few days from her due date, imaging at last showed the devastating discovery—a grapefruit-sized tumor wedged in her chest, obstructing the artery to her right lung. The tumor was suffocating her airway and threateningly restricting oxygen delivery, placing mother and baby alike in danger.
MaKenna was flown to Northwestern Memorial Hospital in Chicago, where she was admitted to the intensive care unit. Within a short time after arrival, she went into labor. Her blood pressure rose, the baby became distressed, and physicians realized that they had only hours—possibly minutes—to move.
"Her lungs were impaired because of the tumor, and labor was also slowing her down to breathe. The danger of respiratory failure and cardiac arrest was very real," said Dr. Lynn Yee, a maternal-fetal medicine specialist at Northwestern Medicine.
MaKenna was put on extracorporeal life support (ECMO)—a life-supporting device that circulates oxygenated blood outside of the body—and received an emergency C-section. Her baby boy, Colter, was delivered safely, healthy in spite of the wild ride he had getting here.
For MaKenna, there was a mix of joy and fear. "Because of the tumor, the delivery came so rapidly. I was mourning the birth plan I had been planning for months, while also coping with the news of my surprise diagnosis," she explained.
What is Rare and Aggressive Melanoma?
After the birth, physicians initiated additional tests. A bronchoscopy test showed the tumor was stage 3 melanoma—a skin cancer that had somehow traveled and developed inside her chest.
This posed a singular challenge. "There isn't much written about or a lot of published cases on how to treat melanoma that comes in this way," said Dr. Kalvin Lung, a thoracic surgeon at Northwestern Medicine. "We had to fall back on the knowledge our team has gained from years of taking care of complex thoracic cases."
Prior to surgery, doctors gave three doses of immunotherapy to shrink the tumor. The therapy was effective in diminishing its size from 13 centimeters to 9 centimeters, thus enabling the subsequent action—surgery.
The procedure itself was extremely complicated. Dr. Lung and Dr. Chris Mehta, a cardiac surgeon with Northwestern Medicine, were required to remove MaKenna's right lung entirely, part of the pulmonary artery, and related lymph nodes. The tumor had invaded large blood vessels and spread throughout all three lobes of the right lung. "We may have a case like this every few years," said Dr. Mehta.
Now 27, MaKenna is stable and continues her immunotherapy treatments. Her scans show no new signs of metastatic cancer, and the tumor site remains inactive. She’s focusing on motherhood, recovery, and gratitude.
“Colter is the best baby—always smiling and sleeping through the night,” she said. “I can’t say enough about the incredible medical team that saved my life. Because of them, I’m here today.”
Dr. Yee continued, "To see MaKenna doing so well, and Colter thriving, brings tears to my eyes. It demonstrates what coordinated, compassionate medical care can do."
Can Pregnancy Shadow Life-Threatening Illnesses?
Pregnancy is commonly accompanied by a variety of physical changes—fatigue, shortness of breath, backaches, nausea, and swelling. Although these symptoms are typically harmless, they sometimes mask the signs of serious underlying medical conditions. This crossover between normal pregnancy pains and signs of potentially fatal diseases can mean that the illnesses are not diagnosed until late, as in the recent case of MaKenna Lauterbach—a 26-year-old woman whose relentless cough and shortness of breath throughout her pregnancy proved to be stage 3 melanoma in her chest.
Shared Symptoms of Pregnancy and Illness Mimic One Another
Most life-threatening conditions have symptoms that are identical to those of pregnancy. Diseases such as heart disease, blood clots, infections, and even cancer may appear with fatigue, chest pain, shortness of breath, or swelling—commonly attributed to normal pregnancy complaints. This similarity results in a diagnostic blind spot.
For example:
- Shortness of breath can be due to increased oxygen demand during pregnancy but can also result from lung disease or heart failure.
- Swelling in late pregnancy is normal but may indicate preeclampsia, kidney disease, or a tumor compressing veins.
- Nausea and vomiting are usual in the first trimester but may also obscure gastrointestinal cancers or liver disease.
Hesitation With Diagnostic Imaging in Pregnancy
One of the greatest difficulties is that physicians tend to shun some diagnostic tests such as X-rays, CT scans, or MRIs during pregnancy in order to avoid exposing the fetus to radiation. Although this prudence is necessary, it can lead to life-threatening delays if a critical condition is suspected but not diagnosed. In MaKenna's situation, imaging was delayed until her symptoms became critical—by that time, a tumor had obstructed large lung arteries.
Immune and Hormonal Alterations Can Speed Up Underlying Disorders
Pregnancy dampens some immune reactions to shield the developing fetus. Yet, this changed immune environment can give rise to or speed up latent diseases like cancer, autoimmune disorders, or infections. Hormonal spikes can also nourish hormone-sensitive tumors, elevating the risk of complications.
Fetal Over Maternal Prioritization in Emergency Situations
During emergencies, choices are frequently made to safeguard the baby—even at the expense of delaying the mother's treatment. This preference can make cases more complex when the mother's declining health impacts fetal welfare directly. Delayed diagnosis or treatment of maternal illness can put both lives at increased risk.
Emotional and Cognitive Biases
Numerous pregnant women—such as MaKenna—will minimize their symptoms, assuming they are just a result of pregnancy demands. There is also a cultural pressure to suffer through pregnancy, and this can cause women not to speak up or seek second opinions when something does not feel right.
Pregnant patients with severe medical issues frequently need treatment from several specialists: obstetricians, oncologists, cardiologists, or pulmonologists. Without an integrated and coordinated effort, important warning signs can be overlooked or insufficiently explored. MaKenna's survival was partly because of the rapid collaboration between maternal-fetal medicine, thoracic surgery, oncology, and intensive care specialists.
Pregnancy never needs to stand in the way of diagnosing and treating potentially life-threatening diseases. Awareness, early investigation, and multidisciplinary care are critical in distinguishing normal pregnancy symptoms from red flags. Pregnant women must always feel confident enough to voice their concerns, clarify the situation, and stand up for their well-being—because, as MaKenna's experience demonstrates, an early diagnosis can save not just one, but two lives.
© 2024 Bennett, Coleman & Company Limited

