
Credits: Canva
US Government Is Erasing Sexual Orientation From Medical Research Findings—What Does It Mean For Healthcare?
Two California researchers have alleged that the US Government health journal instructed them to remove references to gender and sexual orientation from a scientific manuscript that had already been accepted for publication. Their paper examine smoking habits among the youth in the rural areas and was set to be published in Public Health Reports, the official journal of the US Surgeon General and the US Public Health Service.
However, in the blog post, the two researchers Tamar Antin and Rachelle Annechino, revealed that they were asked to delete terms such as "gender", "cisgender" and "equitable" to comply with an executive order signed by President Donald Trump on his first day back in office. The order directs government agencies to eliminate what it calls "gender ideology" from all official publications.
The blog post also included screenshots that suggested deletion of demographic data on sexual orientation. It also included categories like "straight or heterosexual", "gay and lesbian", "bisexual" and "unknown".
A note accompanying the deletions stated: “Per the Executive Order, we cannot include language surrounding gender.”
Rather than complying with the order, the researchers decided to withdraw their paper entirely.
“In normal times, this would never happen,” said Antin, who serves as the director of the Center for Critical Public Health, a California-based research organization. “I have never been asked to censor any articles for publication, nor, to my knowledge, have any of my colleagues ever been asked to censor words, word choice, or remove data from a publication in response to an executive order from the White House. This is extremely unusual.”
The Rise Of Gender Politics in the US
Ever since Trump returned to the White House, gender identity and sexuality have become the key political battleground. His administration has moved to roll back the policies which address gender issues and also policies that promote diversity, equity, and inclusion (DEI) and has targeted LGBTW+ rights in multiple sectors from education to healthcare.
The executive order that he had passed also has led to censorship of researcher's work, as he and the people in his administration believe that gender identity and sexual orientation have been overly politicized.
How Does It Impact Healthcare And Medical Research?
Public health experts stress that including gender and sexual orientation in research is not a political statement but a scientific necessity. These demographic factors play a crucial role in health outcomes, particularly in studies related to smoking, substance use, mental health, and disease prevention.
Antin noted that removing this data could weaken public health efforts. “Understanding how smoking fits into the lives of rural young adults of all genders and sexual orientations can help tailor more effective public health messages,” she explained.
The censorship of such information could have broader implications:
Medical Research Gaps: Without gender and sexual orientation data, researchers may struggle to identify disparities in disease prevalence, mental health risks, or substance use patterns among LGBTQ+ populations.
Policy Decisions: Public health policies could be based on incomplete or misleading data, leading to ineffective interventions.
Funding Challenges: Research grants and funding for LGBTQ+ health issues may decline as federal agencies downplay the importance of gender-related studies.
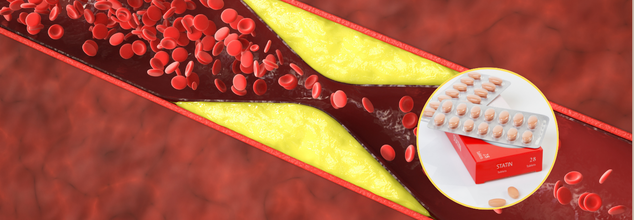
Cholesterol- Lowering And Statin Drug Combo Could Cut Fatalities By 49%, Saving Thousands Of Lives, Study Finds
Cardiovascular diseases remain the number one cause of death across the world, claiming an estimated 18 million lives every year. Although statins have been the first line of treatment for reducing cholesterol levels for years. They achieve this by suppressing an enzyme in the liver that is used to make cholesterol, thus lowering low-density lipoprotein cholesterol (LDL-C), or 'bad' cholesterol. Statins are not enough for some patients, though, and this is where ezetimibe steps in.
According to a study in the Mayo Clinic Proceedings, a combination of two cholesterol-lowering medications—statins and ezetimibe—may save thousands of lives every year by cutting heart attacks, strokes, and other cardiovascular events by half. This study contradicts the traditional practice of prescribing statins alone and recommends the use of combination therapy immediately in high-risk patients.
Ezetimibe has a different mode of action than statins as it inhibits the absorption of cholesterol in the gut, complementing the effect of the statins. The new research uncovers that prescribing both drugs concurrently from the start, instead of adding ezetimibe subsequently, yields considerably superior results for high-risk patients with cardiovascular disease.
The largest study ever conducted, it pooled data from 14 earlier trials involving 108,353 patients. These patients were at 'very high' risk of developing a heart attack or stroke, or had already developed one. The results strongly support the need to modify treatment strategies in high-risk patients.
The study discovered that the patients who underwent the combination therapy had a 19% lower risk of dying from any cause. There was also a 16% decline in cardiovascular death, which pointed to the substantial effect of the therapy on the heart. The study further found that the major adverse cardiovascular events, such as heart attacks and strokes, decreased by 18% and 17%, respectively. These findings reinforce the effectiveness of combining cholesterol-lowering drugs in reducing mortality and preventing life-threatening cardiovascular complications.
LDL-C levels dropped significantly more in those receiving the combination treatment, increasing the likelihood of reaching the target level of under 70mg/dL by 85%.
Traditionally, statins alone have been prescribed for years, and the physician would later evaluate if extra medicine is required. But based on the findings of the study, physicians ought to prescribe the two drugs at once to those patients who are high-risk patients. This change can save more than 330,000 deaths a year across the globe, including almost 50,000 fatalities in the United States alone, says the study's lead author, Prof. Maciej Banach from Poland's John Paul II Catholic University of Lublin.
This study is conclusive that combination cholesterol-lowering therapy must be entertained forthwith and must be the treatment of choice for very high-risk patients following an acute cardiovascular event," said Prof. Peter Toth, one of the authors of the study.
The strategy not only has the potential to save lives but may also lead to substantial cost savings for healthcare systems through decreased hospitalization and complications from untreated cardiovascular disease. Prevention of heart failure, recurrent strokes, and other catastrophic events would reduce the economic burden of long-term cardiac care.
How Does The Drug Combination Affect Treatment for Cardiovascular Diseases?
High levels of LDL-C contributed to 4.5 million deaths in 2020 independently, with most deaths occurring in Eastern Europe and Central Asia. With the prevalent nature of cardiovascular disease worldwide, implementing combination therapy as the mode of treatment might have far-reaching advantages.
Since statins and ezetimibe are already on the market in clinical practice, implementation of these findings should be relatively easy. Scientists hope that this evidence will be followed by a revision of medical guidelines, motivating healthcare professionals across the globe to become more proactive.
The authors of the study emphasize the need for changing current treatment regimes. Doctors are urged to begin patients on combination therapy immediately, and not to wait and observe whether statins alone can work. Immediate and forceful treatment might be the difference between life and death for thousands of people every year.
"Our results emphasize the wisdom of the saying 'the lower the better for longer,' but also the not-less-important 'the earlier the better' in the treatment of high-risk cardiovascular patients," Toth said.
For individuals, this news is a wake-up call to talk with their healthcare provider about cholesterol control strategies. Knowing the value of combination therapy and fighting for full treatment options could have a major impact on long-term health.
The new evidence is a strong argument for the routine application of combination therapy in controlling cholesterol levels for patients at risk. With a solid body of evidence in favor of its application, physicians everywhere are encouraged to implement this treatment to cut the death toll from cardiovascular disease. As guidelines continue to change, the universal use of this practice could be a new dawn for the prevention of heart disease, saving half a million lives each year.
Credits: Canva
FDA Approves Tremfya For Active Crohn's Disease
Of the many things new, the US Food and Drug Administration (FDA) has approved Tremfya (guselkumab) for adult patients with moderately to severely active Crohn's disease.
What is Crohn's Disease?
Crohn's disease is a type of inflammatory bowel disease (IBD) that causes swelling and irritation of the tissues, called inflammation, in the digestive tract. This can lead to belly pain, severe diarrhea, fatigue, weight loss and malnutrition.
What does Tremfya do?
It contains the active ingredient guselkumab, which is a prescription drug to treat moderate to severe plaque psoriasis, psoriatic arthritis, and ulcerative colitis in adults, recently it has been approved for Crohn's disease.
Guselkumab targets the IL-23 subunit alpha which prevents it from binding to cell receptors that would otherwise be activated by its presence. It was first developed by Janseen Pharmaceuticals and in November 2016, a Biologics License Application to FDA was submitted to seek for its approval.
Tremfya blocks interleukin-23 or IL-23, which is a cytokine responsible for inflammation and binds to CD64, which is a receptor on cell that produce IL-23. The CD64 cells are the source of IL-23, which causes inflammation in Crohn's disease.
This approval is the fourth indication for this dual IL-23 inhibitor in the United States, which makes Tremfya the first and only IL-23 inhibitor that offers subcutaneous and intravenous induction options for adults with Crohn's disease.
How Was It Approved?
The approval is based on the data from a 3-phase trial. In the GRAVITI study, 400mg of Tremfya was administered through subcutaneous induction at 0,4,and 8 weeks. This led to a significantly higher clinical remission and endoscopic response when compared with the placebo. The clinical remission was 56% while placebo noted for only 22%, whereas endoscopic response was 35% and placebo had a 15% impact. Similar results were also seen in the second and third phase of trials which compared Tremfya 200mg intravenous induction at weeks 0,4, and 8 with placebo.
"Despite the progress in the management of Crohn's disease, many patients experience debilitating symptoms and are in need of new treatment options," lead investigator of the GRAVITI study, Remo Panaccione, M.D., from the University of Calgary in Alberta, Canada, said in a statement. "Importantly, the fully subcutaneous regimen offers choice and flexibility for patients and providers that have not been available before."
What Are The Symptoms Of Crohn's Disease?
- Diarrhea
- Fever
- Fatigue
- Belly pain and cramping
- Blood in the stool
- Mouth sores
- Reduce appetite and weight loss
- Pain or damage near or around the anus due to inflammation
It can also affect any part of the small or large intestine and could in fact involve multiple segments or may be continuous. It most commonly involves the last part of small intestine. In some people, the disease is only in the colon or the large intestine.
While symptoms of Crohn's disease can range from mild to severe, they usually develop gradually. However, sometimes it may also come suddenly without a warning. So, someone with Crohn's disease may have periods of time without any symptoms, called remission.

Credit: Canva
Tamim Iqbal Suffers Heart Attack-Can It Be Possible To Predict It Beforehand?
Former Bangladesh one-day international (ODI) cricket captain Tamim Iqbal has been hospitalized after he suffered a heart attack on the field during a domestic match. The 36-year-old was leading Mohammedan Sporting Club in a match of the Dhaka Premier League (DPL) on Monday when he complained of chest pain., after which he was rushed to the hospital.
Tariqul Islam, a team official, told a leading media organisation, that Tamim was being treated at a hospital in Savar on Dhaka’s outskirts and urged people to pray for his quick recovery. Meanwhile, the doctors also released an official update wherein they said, "He returned to us in a critical condition. We can call it a heart attack, and we subsequently did an angiogram ( X-ray for blocked arteries) and angioplasty to remove the blockage. The medical procedure has gone smoothly. He is currently under observation. The swift coordination between the medical staff at BKSP and the hospital ensured Tamim was treated quickly."
Can We Predict Heart Attacks?
You can identify a heart attack if the person feels sudden pain or discomfort in the chest, shortness of breath, nausea or sweating. However, several symptoms can occur a month before a person actually suffers a heart attack. They include
1. Chest Pain: A persistent feeling of pressure, tightness, or squeezing in the chest is a hallmark sign that may precede a heart attack.
2. Pain in Other Parts of the Body: Heart attack symptoms aren’t always confined to the chest. Pain may radiate to the arms, jaw, neck, back, or stomach, often described as an aching or heavy sensation.
3. Shortness of Breath: Struggling to catch your breath or feeling out of breath without significant exertion can indicate reduced blood flow to the heart and lungs.
4. Unusual Fatigue: Feeling excessively tired, even after minimal effort, could be a subtle sign of heart trouble.
Why Is Angioplasty Done?
Angioplasty is a procedure that widens blocked or narrowed arteries. It restores blood flow to the heart without open heart surgery. For angioplasty, a long, thin tube (catheter) is put into a blood vessel. It is then guided to the blocked coronary artery. The catheter has a tiny balloon at its tip. Once the catheter is in place, the balloon is inflated at the narrowed area of the heart artery. This presses the plaque or blood clot against the sides of the artery. The result is more room for blood flow.
In recent times, incidences of people suffering from heart attacks while being in the middle of an activity that is physically exerting like running on treadmills, have been repeatedly reported. Iqbal already had blockages in his heart when he was on the field. There is a huge probability that this caused his heart attack.
© 2024 Bennett, Coleman & Company Limited

