- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories

Assisted Dying (Credit: Canva)
UK Presents Bill To Allow 'Assisted Dying': What It Means And How Is It Different From Euthanasia
Terminally ill people in England and Wales could have the right to choose to end their life—a practice that is already legal in a few countries. Earlier this month, Labour MP Kim Leadbeater introduced the Terminally Ill Adults (End of Life) Bill, which was voted upon recently. A separate but similar bill is under discussion in Scotland.
What Is Assisted Dying?
Put in simple terms, it refers to the practice of ending a person's life through medication—either self-administered or by a medical professional. Assisted death is legal in at least 11 states across the US along with a handful of other countries like Canada and Belgium. It is important to note that assisted dying includes both assisted suicide and euthanasia.Assisted suicide is intentionally helping another person to end their life, which may not even require a terminal diagnosis but again it depends from place to place and condition to condition. That could involve providing lethal medication or helping them travel to another jurisdiction to die. However, the bill presented in UK clearly states that it will be used only for patients who are terminally ill and have less than 6 months to live.
How Is It Different From Euthanasia?
Euthanasia—also referred to mercy killing—is the practice of intentionally ending a life to relieve pain and suffering. The legality of this practice varies across the globe, with a small number of countries permitting it under strict conditions. The list include Belgium, Australia, Canada, Colombia, Ecuador, Luxemburg, The Netherlands, New Zealand, Portugal and Spain.
At present, laws throughout the British territory prevent people from asking for medical help to die. However, the bill could change it. Here are the requirements of the proposed bill:
Anyone who wishes to end their lives, must be over 18 and live in England and Wales, and have been registered with a GP for at least 12 months
They must have the mental capacity to make the choice and be deemed to have expressed a clear, settled and informed wish, free from coercion or pressure
They will be expected to die within six months
Also, they need to make two separate declarations, witnessed and signed, about their wish to die
Finally, they need to satisfy two independent doctors that they are eligible - with at least seven days between each doctors' assessment
Moreover, a High Court judge must hear from at least one of the doctors, and can question the dying person, or anyone else considered relevant. After the judge has made their ruling, a patient would have to wait another 14 days before acting. Notably, it is completely illegal to pressurize someone to take their own lives. Anyone found to do could risk a 14-year prison sentence.
The bill is also facing considerable opposition. Opponents reportedly argue that legalizing assisted suicide could pressure vulnerable individuals into ending their lives. They urge the government to prioritize enhancing palliative care instead. Among those opposing the change is Paralympian and House of Lords crossbencher Baroness Grey-Thompson, who has voiced concerns over the potential risks of altering the law on assisted death.
Is It Different in Scotland?
Yes, the bill is slightly different in Scotland. A person calling for assisted suicide must be a resident of the country for at least 12 months. Additionally, they should be registered with a GP in Scotland, be terminally ill and must have the mental capacity to make the request.
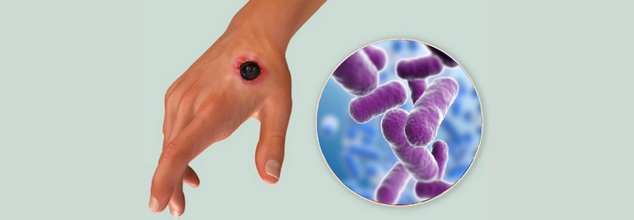
Thailand Confirms First Anthrax Death In 30 Years Raises Alarm Over Potential Spread
Thailand's health officials reported on Wednesday the first human anthrax death since 1994, a tragic first in the northeastern province of Mukdahan. A 53-year-old man who had slaughtered and eaten raw beef developed cutaneous lesions and systemic symptoms before dying from infection despite being treated. Another case was confirmed in a friend with the same exposure, and three more suspected cases are being investigated. This unusual death has triggered an emergency public health response from several government agencies.
Anthrax is caused by the spore‑forming bacterium Bacillus anthracis, which mainly infects grazing livestock and wildlife. Humans become infected by direct contact with infected animals, contaminated animal products, or by eating undercooked meat. There are three clinical forms:
Cutaneous anthrax, the most prevalent, develops from itchy papules, which become black eschars, and is usually lethal if untreated.
Gastrointestinal anthrax, caused by the ingestion of tainted meat, causes acute pain in the abdominal area, nausea, and hemorrhagic diarrhea.
Inhalational anthrax—isolated, yet fatal—is produced when the spores are breathed in and manifest as respiratory insufficiency and systemic shock.
Unlike most infectious diseases, anthrax is not transmitted person-to-person. Early antibiotic treatment is effective, but delay in diagnosis can permit the bacteria to spread and cause life-threatening illness.
All About the Mukdahan Outbreak
The epidemic hub was in Don Tan district, Mukdahan Province, literally on the other side of the Mekong River from Laos, where 129 cases of anthrax (one fatal) were reported during the last year. Thai authorities have tracked down 638 people possibly exposed via butchering or eating raw beef: 36 butchers and 602 consumers are now being closely monitored and administered prophylactic antibiotics
Dr. Weerawat Manosuthi, Thailand's Disease Control Department spokesman, reported, "All those who are suspected to have come into contact with contaminated meat are under observation," emphasizing the need for expedient containment measures to avoid further infections.
Following the death and second confirmed case, Thailand's Agriculture Ministry has declared a 5‑kilometer cordon of quarantine around the animal exposure site. In this cordon, 1,222 cattle will be vaccinated by the Livestock Department, although none have as yet shown signs of disease or unexplained death
In the meantime, all suspected human contacts are on a course of ciprofloxacin or doxycycline, under close observation for the first symptoms of the disease. Clinics have been set up to identify anthrax signs, including painless ulcers on the skin and swollen lymph nodes, and to provide quick diagnostic tests, such as PCR assays.
Anthrax is also endemic in Southeast Asia, and border states have recently struggled with outbreaks as well. Laos's outbreak in 2024 and Vietnam's 13 cases reported in May 2023 underscore the impermeable nature of zoonotic disease transmission across the region. Thai health officials are meeting with their colleagues in Laos, Cambodia, and Vietnam to exchange information and coordinate surveillance efforts along borders.
Dr. Narong Chankaeo, head of the Mukdahan provincial health department, cautioned that environmental conditions—like flooding which exposes spores to the surface—could cause future outbreaks. "Increased surveillance in border towns and among cattle handlers is a must," he said.
Why Anthrax Reemerges?
In Mukdahan, the eating of raw beef dishes is a cultural norm that adds to risk. Flooding during certain seasons can disrupt spores hidden beneath the soil, infecting pastures and water sources. Added to unregulated butchering practices—frequently without protective equipment—these create a perfect storm for the reemergence of anthrax.
Experts also point out that years without a fatal case could have bred complacency both among the public and veterinarians. Dr. Saneemongkol Sawettanan, an epidemiologist at Bangkok's Ministry of Public Health, added, "We need to retrain rural health workers and farmers of livestock about anthrax prevention—lapses in awareness can be fatal."
From Rapid Response to Long‑Term Prevention
Although Thailand's rapid quarantine and vaccination campaign are essential initial actions, long‑term prevention involves a One Health strategy—aligning human, animal, and environmental health initiatives. These are:
- Routine cattle vaccination in areas of high risk
- Public awareness on proper meat handling
- Surveillance of anthrax spores in water and soil
- Exchange of data across borders and joint simulation of outbreaks
Through an improvement in veterinary services and public health infrastructure, Thailand can decrease the chances of future deaths.
Thailand’s first anthrax death in three decades is a stark reminder that even well‑known pathogens can re‑ignite under conducive conditions. As global travel and trade resume post-pandemic, zoonotic threats remain ever‑present. The Mukdahan outbreak underscores the importance of:
- Maintaining robust vaccination programs for livestock
- Ensuring rapid diagnostic capacity at local clinics
- Fostering regional collaboration on disease surveillance
- Balancing cultural practices with food safety education
What is Anthrax?
Anthrax is an uncommon but sometimes life-threatening illness caused by the spore-forming bacterium Bacillus anthracis that is naturally distributed in soil. Although it only infects animals and wild animals, humans are at risk when they have direct or indirect exposure to infected animals or contaminated animal products.
Unlike most contagious diseases, anthrax is not directly spread from human to human. Yet, skin sores from anthrax do carry a slight risk if a person touches them or contaminated objects (fomites) directly. The majority of human infections happen when bacterial spores gain entry into the body through cuts in the skin, eating undercooked contaminated meat, or through inhaling airborne spores.
Symptoms to Know
There are four major forms of anthrax infection, each having different symptoms. Incubation usually lasts between one to six days, but inhalation anthrax can take weeks to appear.
Cutaneous Anthrax (Skin-Related)
This is the most frequent and least deadly form of anthrax. It happens when the bacteria get into the body through a cut or scratch on the skin. If medical treatment is sought soon enough, cutaneous anthrax seldom develops life-threatening complications.
Common signs and symptoms are:
- A small, itching bump that looks like an insect bite and soon develops into a painless ulcer with a black center
- Swelling around the infected sore
- Swollen lymph nodes near the infection site
- At times, flu-like signs and symptoms like fever or headache
When Should You Seek Medical Attention?
Since initial anthrax symptoms may be similar to those of run-of-the-mill viral infections—such as the flu—it's simple to miss the early warning signs. But if you suspect exposure, particularly in a work environment where contact with infected animals or animal by-products may occur, immediate medical assessment is paramount.
Consult a doctor immediately if you experience strange skin lesions, fever, or respiratory disease following exposure in areas where anthrax infection is known to exist. Early treatment with antibiotics can make a big difference.

Credits: Canva
CDC Reports 216 Child Deaths From Flu This Season, The Worst Since Swine Flu Outbreak
The Centers for Disease Control and Prevention (CDC) has officially reported the largest number of pediatric deaths in more than 15 years, topping even last year's death count and paralleling the killing impact of the 2009-2010 swine flu pandemic. At least 216 U.S. children have lost their lives from influenza-related causes through the current 2023–2024 flu season as of early May, a count that experts cautioned will likely still grow as further data are accumulated.
Dr. Sean O'Leary, a pediatric infectious disease physician at the University of Colorado and a spokesperson for the American Academy of Pediatrics, noted that the reported death toll is probably an underestimation. "This number that we have now is almost certainly an undercount," he said in an interview with the Associated Press, adding that final counts from CDC flu data are usually revised and finalized during the fall.
One of the most disturbing factors contributing to the surge in child flu deaths is the dramatic decline in rates of flu vaccination among children. The vaccination rate has plummeted from 64% five years ago to only 49% this flu season, reports Dr. O'Leary. The seriousness of the decline cannot be overstated—particularly with the fact that flu vaccines, though they cannot always prevent illness, are shown to significantly reduce the risk of hospitalization and death.
The information indicates that a majority of the deaths were preventable. The number of children who received vaccinations among the 216 that passed away was not released by the CDC, nor did they provide expert insight within the report. Nevertheless, it is hard to ignore the trend between declining flu vaccine usage and higher mortality.
Adults were not exempt from this year's flu season either. The CDC estimates that this season's flu has sickened at least 47 million people, hospitalized 610,000, and killed 26,000 in all ages up to this point. In adults who were hospitalized with flu, 95% had one or more underlying conditions, including diabetes or heart disease. But the scenario is very different among children: only around 53% of the nearly 2,000 hospitalized children researchers examined had an underlying condition, including asthma or obesity. This means many of the sickened children were otherwise well.
These kinds of statistics confirm the capricious and sometimes indiscriminate nature of the flu virus—especially in years when several aggressive strains are in circulation at the same time.
Why This Year Was Particularly Challenging?
The season of 2023–2024 has been peculiar when it comes to virology. Rather than a single prevalent strain, two distinct Type A strains—H1N1 and H3N2—have been spreading extensively, making it even more complex in terms of diagnosis, treatment, and prevention. Fortunately, the flu vaccine has been working fairly well, based on previous CDC information that indicated that it was efficient in cutting down hospitalizations and deaths.
Nevertheless, a large number of Americans did not get vaccinated or got vaccinated too late. Misinformation, logistical challenges, and decreased access to pediatric vaccination services have all contributed.
The healthcare infrastructure also has a part in these results. As Dr. O'Leary noted, pediatrician clinics nationwide are running short on staff and are seeing fewer after-hours clinics, which makes it harder for families to get their children vaccinated. Although pharmacies have become the default choice for many adults who are seeking vaccines, they are not all equipped—or even permitted by law—to vaccinate children.
This access structural gap is an increasingly pressing concern, particularly as more Americans are turning to retail healthcare environments for routine vaccinations.
Why is Vaccine Hesitancy and Political Rhetoric a Dangerous Mix?
Superimposed over this entire crisis is a general collapse in childhood vaccination rates across the board—led in part by a steady stream of misinformation online and amplified by political leaders. Robert F. Kennedy Jr., now the U.S. Secretary of Health and Human Services, publicly sided with vaccine-critical language, which restarted debates that swept up speed during the COVID-19 pandemic. His divisive stance is thought to have impacted public trust and potentially led to a general collapse in vaccine confidence.
Experts fear that this politicization of public health measures may be eroding decades of effort in infectious disease prevention.
Flu Activity Now in Decline
There is some relief: the CDC says flu activity is now declining, with all 50 states reporting low or minimal levels. But for the families of the 216 children who died this season, it comes too late.
Public health officials continue to strongly recommend annual flu vaccinations for everybody six months and older, warning Americans not to get complacent. "My hope is that this season will be a little bit of a wake-up call," said Dr. O'Leary. "We actually do need to vaccinate our kids against influenza."
The increase in pediatric flu fatalities in the 2023-24 season is a failure of public health with several contributing layers—vaccine hesitancy, systemic gaps in healthcare, and politicization of science. And yet, it's also an moment of clarity. Influenza is a serious, occasionally fatal virus, and vaccines are among our most effective weapons in limiting its spread.
As flu season comes to a close, the call to action is clear: heightened awareness, greater vaccine availability, and a collective effort to restore trust in public health must be top priorities to avoid another tragic year.

Credit: Canva
Many Vegans Miss Out On Key Amino Acids Despite Getting Enough Protein, Study Reveals
YourA new study has found that while many long-term vegans consume enough total protein daily, a significant number still fall short of essential amino acids, raising concerns about protein quality in plant-based diets.
Conducted by a team of nutritionists from Massey University in New Zealand, the research analysed the diets of 193 vegans using four-day food diaries. The team used data from the U.S. Department of Agriculture and the New Zealand FoodFiles database to estimate amino acid intake from various plant-based foods. Their findings, published in the journal PLOS One, shed light on the challenges vegans face in achieving complete protein nutrition.
According to the study, around 75% of participants met their total daily protein needs. However, only about half reached the required intake for two crucial amino acids—lysine and leucine. These amino acids are classified as "indispensable" because the human body cannot produce them on its own and must obtain them through diet.
“Meeting adequate total daily protein intake in a vegan diet does not always guarantee a high protein quality diet,” the researchers warned. “Simply considering total protein intake without evaluating protein quality may lead to an overestimation of nutritional adequacy among vegans.”
Lead researchers Bi Xue and Patricia Soh emphasized the importance of including a diverse range of plant foods to meet the full spectrum of amino acid needs. While the body can synthesize many amino acids, nine must be sourced directly from food—making dietary balance crucial, especially in vegan diets.
The study pointed to legumes, nuts, seeds, and soy products as valuable sources for boosting lysine and leucine intake. These plant-based options can help vegans meet both their total protein requirements and maintain the right amino acid profile necessary for overall health.
“Achieving high protein quality on a vegan diet requires more than just consuming enough protein,” the team noted. “It also depends on the right balance and variety of plant foods to supply all the amino acids in the quantities our body needs.”
The researchers concluded by calling for further studies to explore effective strategies for improving amino acid intake in vegan populations. As more people adopt plant-based lifestyles, understanding how to maintain both protein quantity and quality is becoming increasingly important for public health.
Do you want a headline suggestion or social media blurb for this article?
© 2024 Bennett, Coleman & Company Limited




