Most Common Vaginal Infection May Actually Be An STD, Study Finds
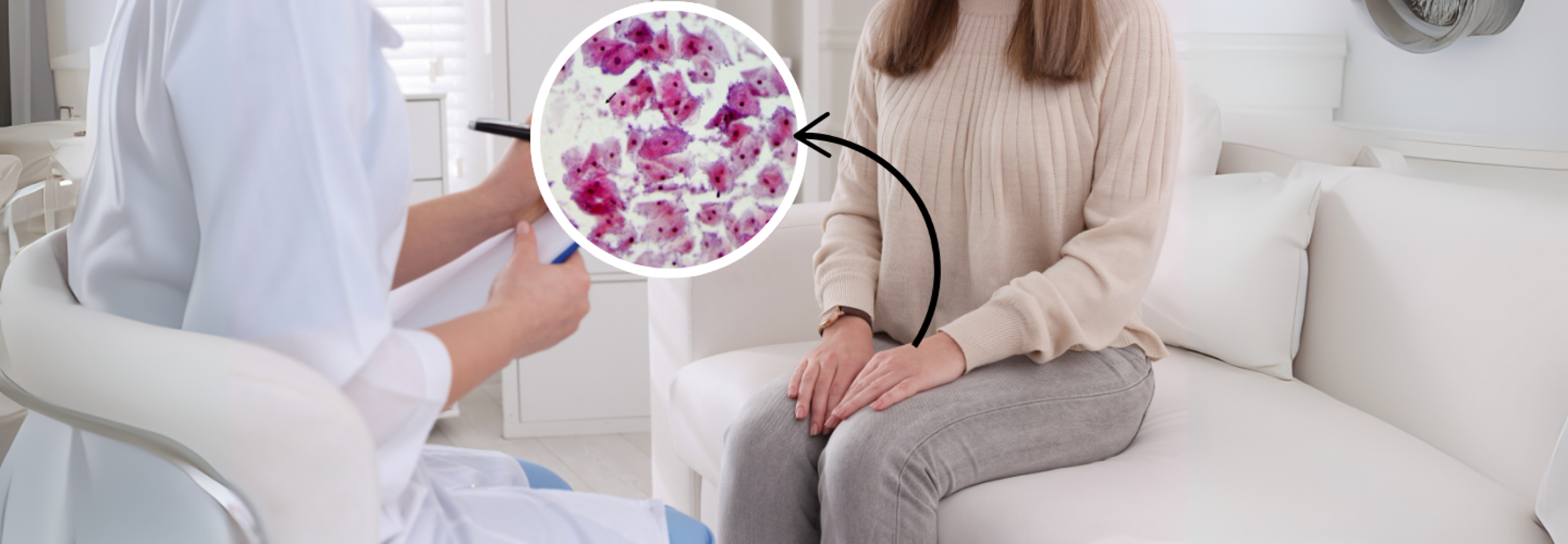
SummaryBacterial vaginosis (BV), the most common vaginal infection, may be sexually transmitted, with studies showing that treating male partners significantly reduces recurrence rates in women.
End of Article
