- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Measles Outbreak Cases Cross 100 Mark In US, Australia Sees Sudden Surge Of The Infectious Disease

(Credit-Canva)
The current measles outbreak has gripped US states like Texas and New Mexico leaving people worried whether it would become a new pandemic. According to the Texas Department of State Health Services as of February 21, 90 cases were diagnosed in the last month in the South Plains area, with at least 77 of them were reported in children and teens under 17.
Measles is highly contagious and can be deadly. The outbreak, which started spreading in late January, has resulted in multiple hospitalizations, with at least nine confirmed cases and three probable cases as of early February. Health officials caution that at least one in five infected individuals will have to be hospitalized, highlighting the severity of the situation.
Misinformation surrounding vaccines and with the new Trump administration anti-vaccine campaigs, has causing parents to hesitate or refuse vaccination.
Furthermore, the country down under Australia is also witnessing a surge in measles cases as health officials in Sydney have issued an urgent alert, urging residents to watch for measles symptoms after an infected individual visited several places in Sydney over the last seven days.
Authorities report that the traveller had returned from South East Asia where there are ongoing outbreaks of measles.
What Are The Symptoms Measles?
Key symptoms of measles include fever, a runny nose, sore eyes, and a cough. Typically, a red, blotchy rash appears three to four days later, spreading from the head down to the body. Symptoms can manifest between 7 and 18 days after exposure.
Anyone who experiences these symptoms after potential exposure should immediately contact their doctor or emergency department. It is crucial to call ahead before visiting to avoid potentially exposing others in the waiting room. Dr. Selvey also highlighted that ongoing measles outbreaks are occurring in various parts of the world, making awareness and prompt action essential.
Why It Is Important To Get Vaccinated?
According to CDC everyone should get the MMR vaccine. It protects you from measles, mumps, and rubella. Getting vaccinated helps stop these diseases from spreading. There are two safe MMR vaccines available. They work the same way, so it doesn't matter which one you get. Kids can also get a shot that protects against chickenpox too, but this is only for children.
Who Should Get Vaccinated?
Kids Need Two Shots
All children should get two MMR shots. The first shot should be given when they are between 12 and 15 months old. The second shot should be given when they are between 4 and 6 years old. If needed, the second shot can be given earlier, but it must be at least 28 days after the first shot.
College Students Need to Be Protected
Students going to college or other schools after high school, need two shots if they are not already immune. The shots must be at least 28 days apart.
Adults Need at Least One Shot
Most adults need at least one MMR shot. Some adults need two shots, especially those who work in healthcare, travel a lot, or go to college. These people should get two shots, with 28 days between them.
Travelers Need to Be Extra Careful
Anyone traveling to other countries should make sure they are protected. Babies 6 to 11 months old should get one shot before traveling. Kids 12 months and older, teens, and adults need two shots, with 28 days between them.
Healthcare Workers Must Be Immune
People who work in healthcare should have proof that they are immune to measles, mumps, and rubella. If they are not immune, they need two MMR shots, spaced 28 days apart.
Women Thinking About Having Babies
Women who might get pregnant should talk to their doctor about the MMR vaccine. It's safe to get the shot while breastfeeding.
India Saw Over 1.5M Cancer Cases In 2025: Which States Are Worst Hit?

Credit: Canva
India has seen a significant rise in the cancer burden, with the cases rising to 1,569,793 in 2025, the government has informed the Parliament.
From more than 1.4 million in 2021, the cancer cases in the country rose to over 144,000 in the last five years, revealed Prataprao Jadhav, Union Minister of State for Health, in a written reply in the Rajya Sabha.
The increase in cases has been consistent:
- 1,426,447 cases in 2021
- 1,461,427 cases in 2022
- 1,496,972 cases in 2023
- 1,533,055 cases in 2024
- 1,569,793 cases in 2025
Similarly, cancer deaths also increased in the country -- 868,588 in 2025 from 789,202 in 2021.
The country reported about 15,000 cancer -related deaths each year:
- 789,202 deaths in 2021
- 808,558 deaths in 2022
- 828,252 deaths in 2023
- 848,266 deaths in 2024
- 868,588 deaths in 2025
Worst-Affected States And Key Reasons
Jadhav informed that bigger states with large populations have seen a major increase in cancer cases and deaths consistently in the last five years.
States with the highest estimated cancer cases in 2025 include:
Uttar Pradesh - 226,125
Bihar - 118,136 cases
West Bengal - 121,639 cases
Maharashtra - 130,465 cases
Rajasthan - 80,628 cases
States with the highest estimated cancer deaths in 2025 include:
Uttar Pradesh - 125,184 deaths
Bihar - 65,571 deaths
West Bengal - 67,093 deaths
Maharashtra - 71,696 deaths
Rajasthan - 44,402 deaths
Major reasons for the rise in cancer burden include:
- environmental factors such as industrial pollution, pesticide exposure,
- contaminated water sources, by pollutants like industrial waste, pesticides, heavy metals, and pharmaceuticals.
“The review provides a critical analysis of the current evidence, summarizing the association of water contamination, including industrial waste, pesticides, and heavy metals, with rectal and colorectal cancer,” Jadhav stated in the Upper House of the Parliament.
Cancer Care Facilities In India
Jadhav further informed that the government is tackling the growing burden by expanding cancer care infrastructure across the country.
The Ministry of Health and Family Welfare has implemented the Strengthening of Tertiary Care Cancer Facilities Scheme, which has approved:
- 19 State Cancer Institutes (SCI)
- 20 Tertiary Care Cancer Centers (TCCC)
Other high-quality comprehensive cancer care facilities in the country include:
- Tata Memorial Centre’s (TMC) six hospitals in Varanasi, Visakhapatnam, New Chandigarh, Guwahati, Sangrur, and Muzaffarpur
- Cancer treatment facilities in all 22 new AIIMS
- Advanced diagnostic and treatment facilities at the National Cancer Institute (NCI) at Jhajjar
- A second campus of Chittaranjan National Cancer Institute in Kolkata
- 297 Day Care Cancer Centers (DCCCs) as promised in the Union Budget 2025-26
- Free essential medicines and diagnostics at public health facilities
- Anti-cancer drugs in the Essential Drugs List at District and Sub-Divisional Hospitals
- Health insurance of Rs. 5 lakh per family annually for secondary and tertiary care under Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB PMJAY)
- Affordable Medicines and Reliable Implants for Treatment (AMRIT) Pharmacies providing access to affordable cancer medicines.
New dengue vaccine over 80% effective, prevents severe disease for up to 5 years
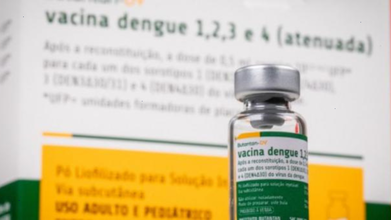
Credit: Butantan Institute
A new vaccine that targets the mosquito-borne dengue has proven to be over 80 percent effective in preventing the risk of severe disease for up to five years, according to a recent study conducted by Brazilian researchers.
The study, published in the journal Nature Medicine, confirmed that the tetravalent dengue vaccine -- Butantan-DV -- developed by the Butantan Institute in São Paulo, prevents hospitalizations and offers broader protection against all four dengue serotypes.
“This vaccine is establishing itself as a very important tool in the fight against dengue in Brazil, with the potential to contribute to reducing the circulation of the virus, in addition to individual protection,” said Fernanda Boulos, the institute’s medical director of clinical trials.
The Phase 3 Clinical Trial
The phase 3 clinical trial, conducted from February 2016 to July 2019, involved 16,235 participants between the ages of 2 and 59.
The researchers compared individuals who received a single dose of the vaccine (10,259) with those who were administered a placebo (5,976).
- The results showed
- 80.5 percent effectiveness against severe dengue cases
- no hospitalization in the vaccinated group vs 8 cases in the placebo group
- 65 percent effective in preventing symptomatic dengue
The Butantan-DV Vaccine
The Butantan-DV vaccine is tetravalent and offers protection against the four known serotypes: DENV-1, DENV-2, DENV-3, and DENV-4.
The vaccine uses live viruses that have been “weakened” (attenuated) in a laboratory.
Once administered, the vaccine controls replication of these attenuated viruses in the body -- a process which induces the immune system to produce neutralizing antibodies specific to each of the four serotypes.
The vaccines create immunity specific to each serotype to enable the body to recognize and neutralize each variant individually.
The Butantan-DV vaccine was approved by the Brazilian Health Regulatory Agency (ANVISA) on November 26, 2025, for use by the Brazilian population aged 12 to 59.
The country's Ministry of Health has
- incorporated the vaccine into the national immunization program in January
- launched a pilot project to immunize 90 percent of the target population in states with high burden
- rolled out vaccination of primary care health professionals in February
Also read: Why Is Dengue Fever on the Rise Despite Vaccines?
Global Dengue Burden
Dengue is transmitted through infected mosquitoes, primarily the species Aedes aegypti.
Common Symptoms include:
- Sudden onset of high-grade fever.
- Intense headache
- Severe muscle, joint, or bone pain.
- Skin Rash that often appears 2–5 days after the fever starts
- Nausea and Vomiting
- Fatigue
According to the World Health Organization (WHO), about half of the world's population is now at risk of dengue.
It estimates that:
- about 390 million dengue infections occur annually worldwide
- nearly 100 million people develop symptoms each year
The two main authorized vaccines in the world against dengue are Dengvaxia and Qdenga.
These vaccines are designed to protect against all four serotypes of the virus, with a focus on reducing severe disease and hospitalizations.
Passive Euthanasia: Harish Rana Case A Compassionate Step In Indian Healthcare

Credit: iStock
The recent decision by the Supreme Court of India allowing withdrawal of life support for a 32-year-old man in an irreversible permanent vegetative state is an important development in patient-centered healthcare.
The order follows the principles established in the landmark Common Cause v. Union of India, which recognized passive euthanasia and affirmed that individuals have the right to die with dignity. From the perspective of a critical care specialist, this decision supports ethical medical practice while protecting the dignity and rights of patients.
In modern intensive care units (ICUs), doctors use advanced technologies such as ventilators, feeding tubes, dialysis machines, and strong medications to sustain life during serious illness. These treatments are extremely valuable when there is a reasonable chance of recovery.
However, in some medical conditions—particularly severe brain injuries—patients may enter a permanent vegetative state. In this condition, the patient’s body may continue functioning with medical support, but the brain has lost the ability to produce consciousness or awareness. The patient cannot communicate, recognize loved ones, or interact with the environment, and medical science currently has no effective treatment to reverse this condition.
From a medical standpoint, continuing life support in such cases may only prolong biological survival without any possibility of recovery or meaningful quality of life. The Supreme Court’s decision acknowledges this difficult reality and allows withdrawal of life-sustaining treatment when doctors confirm that recovery is medically impossible. This approach respects the patient’s dignity and avoids unnecessary prolongation of suffering.
Harish Rana Case: Key benefits
One of the key benefits of this judgment is the recognition of dignity at the end of life. The Court has interpreted the right to life under the Constitution of India to include the right to die with dignity. In practical terms, this means that patients should not be forced to remain on life-support machines when such treatment no longer benefits them.
Medicine should focus not only on prolonging life but also on ensuring that patients are treated with respect, comfort, and compassion during their final stages of life.
The decision also supports patient autonomy, which is a core principle of ethical medical care. Individuals have the right to make decisions about their own bodies and medical treatment. The recognition of living wills or advance directives allows patients to express their wishes in advance regarding life-prolonging treatments. This ensures that medical decisions align with the patient’s values and preferences, even if the patient is no longer able to communicate.
Also read: Harish Rana Case Highlights Why Planning For A Living Will Is Important
Another important benefit is the support it provides to families. Families often experience deep emotional stress when a loved one remains in a permanent vegetative state for a long period. They may struggle with uncertainty about whether continuing life support is truly helping the patient.
The Supreme Court’s framework provides a clear and compassionate process for decision-making involving medical boards and proper documentation. This helps families make informed choices in consultation with doctors while ensuring that the decision is ethically and legally sound.
Harish Rana Case: Offers Clarity For Healthcare Workers
The ruling also offers legal clarity for doctors and hospitals. In the past, physicians sometimes feared legal consequences if life support was withdrawn, even in medically futile situations.
The guidelines established under the Common Cause judgment create a structured and transparent process for making such decisions. This allows doctors to practice responsible and ethical medicine without unnecessary legal concerns.
Also read: Passive Euthanasia: Harish Rana’s Case May Reshape End-of-life Protocols, Say Experts
Passive Euthanasia: A Compassionate Step
In conclusion, the Supreme Court’s order is a compassionate step forward in Indian healthcare. From a critical care perspective, it respects patient dignity, supports family decision-making, provides legal clarity for doctors, and encourages thoughtful end-of-life care.
Most importantly, it reminds us that the true goal of medicine is not merely to extend life at all costs, but to ensure that every patient is treated with dignity, humanity, and respect throughout all stages of life.
Also read: Harish Rana Case Brings Spotlight On How Passive Euthanasia Has Evolved Over The Years
© 2024 Bennett, Coleman & Company Limited

