Credit: Canva
Measles Cases Double In US: Should You Get The Vaccine Now?
US now has more than double the number of measles cases it saw in all of 2024, with Texas reporting another large jump in cases and hospitalizations on Friday. Other states with active outbreaks — defined as three or more cases — include New Mexico, Kansas, Ohio and Oklahoma. The virus has been spreading in 'undervaccinated' communities, and since February, two unvaccinated people have died from measles-related causes.
The multi-state outbreak confirms health experts' fears that the virus will take hold in other U.S. communities with low vaccination rates and that the spread could stretch on for a year. The World Health Organization said last week that cases in Mexico are linked to the Texas outbreak.
Should You Get The Measles Booster Shot?
Measles is caused by a highly contagious virus that's airborne and spreads easily when an infected person breathes, sneezes or coughs. It is preventable through vaccines and has been considered eliminated from the U.S. since 2000.
The best way to avoid measles is to get the measles, mumps and rubella (MMR) vaccine. The first shot is recommended for children between 12 and 15 months old and the second between 4 and 6 years old.
People at high risk for infection who got the shots many years ago may want to consider getting a booster if they live in an area with an outbreak, said Scott Weaver with the Global Virus Network, an international coalition. Those may include family members living with someone who has measles or those especially vulnerable to respiratory diseases because of underlying medical conditions.
Adults with “presumptive evidence of immunity” generally don’t need measles shots now, the CDC said. Criteria include written documentation of adequate vaccination earlier in life, lab confirmation of past infection or being born before 1957, when most people were likely to be infected naturally.
A doctor can order a lab test called an MMR titer to check your levels of measles antibodies, but health experts don't always recommend this route and insurance coverage can vary. Getting another MMR shot is harmless if there are concerns about waning immunity, the CDC says.
People who have documentation of receiving a live measles vaccine in the 1960s don’t need to be revaccinated, but people who were immunized before 1968 with an ineffective measles vaccine made from “killed” virus should be revaccinated with at least one dose, the agency said. That also includes people who don’t know which type they got.

(Credit-Getty Images/Canva)
Bryan Johnson Calls Attention To India’s Deteriorating Air Quality: “I Was Shocked At How Indians Have Normalized This”
Known for being a pioneer in the anti-aging technology, millionaire Bryan Johnson calls out the poor air quality in India and how it is a threat to health and longevity of people in the country. He posted about this previously as well on other social media platforms like X, recalling his first time in India.
His post on X speaks about the declining AQI of the country as the numbers keep climbing higher and higher as years go by. “I was shocked by how normalized Indians are to poor air quality. Breathing the air is like smoking multiple cigarettes a day. Yet no one wears a mask or has air filters in their indoor environments.”
People In India Are Used To Terrible Living Conditions
Bryan, who is famous for trying to reverse aging with special diets and treatments, said that clean air is the most important thing for being healthy. He wondered how people are supposed to focus on being well when the air they breathe is dangerous. Johnson said that the bad air quality was one of their biggest worries about coming to India. He thinks India might have the worst air in the world right now and is surprised that people aren't wearing masks. He said the air feels "awful," like being in the middle of a fire.
Why Does India Need To Prioritize Improving Air Quality?
The poor air quality in India even directly impacted Bryan Johnson's activities during his visit. While he was in Mumbai in February, the air in the room where he was recording a podcast with Nikhil Kamath, a co-founder of a company called Zerodha, was so bad that he had to leave. He later explained that the room was circulating the polluted outdoor air, which made his personal air purifier useless. He also noted that his body reacted negatively, developing a rash and a sore throat after just three days of being in the city, further illustrating the immediate health effects of the pollution.
Delhi's Air is Terribly Polluted Compared to Safe Levels
According to a report from Clean Air Fund, the capital city of India, New Delhi, has the unfortunate title of being the most polluted capital city across the entire globe. The levels of very small and harmful particles in the air, known as PM2.5, are nearly ten times higher than the safety limits recommended by the World Health Organization.
Has The Air Quality Here Gotten Worse?
The AQI is measured on a scale of 0 to 500 with air quality from 0 to 50 considered "good," 51 to 100 - "okay," 101 to 200 - "not good for sensitive people," 201 to 300 - "poor," 301 to 400 - "very poor," and 301 to 500 - "severe". An AQI in the highest range means it's a health emergency for everyone.
Recently, the air quality in Delhi got worse again. After being at a "moderate" level last week, it went back to being "poor" again.
How Does Prolonged Exposure To Pollution Affect Our Health?
According to the World Health Organization (WHO), breathing polluted air increases our risk of dying from all sorts of causes and also leads to specific illnesses. The diseases that scientists have most strongly linked to air pollution include strokes, heart problems, long-term lung diseases, lung cancer, pneumonia, and even cataracts but this is mostly from pollution inside homes.
There's also some evidence suggesting that air pollution might increase the risk of problems during pregnancy like babies being born too small or too early, other types of cancer, diabetes, problems with thinking, and diseases of the brain and nerves. It is important to take necessary precaution like wearing masks outside, having air purifiers and reducing any plans to travel on days when AQI is severe.

(Credit-Canva)
Air Pollution Could Be Causing Cognitive Decline Among Senior Citizens
Air pollution has become a rampant issue, and the health issues that come along with it have also increased. While we know poor air quality can lead to issues like respiratory illnesses, a new study has shown that this pollution may also affect a person's cognitive health as well.
The World Health Organization explains that the presence of dust, fumes, gas, mist, smoke or vapor can be dangerous for a human being’s health. They can cause issues like inflammation, oxidative stress, immunosuppression, and mutagenicity in cells. These can affect one's heart, lungs or brain, eventually leading to failure.
A new study published in The Journals of Gerontology: Series A, indicates that breathing polluted air might be bad for the brains of older adults. The study suggests that being exposed to pollution could make seniors more likely to develop problems with their thinking and memory, possibly even increasing their chances of getting dementia. This research adds important information to our understanding of how the environment can affect the health of our brains as we get older.
What Components Of Pollution Is Linked To Cognitive Decline?
The researchers found a clear connection between older people being exposed to two types of air pollution – nitrogen dioxide and very small particles in the air – and them doing worse on tests that measured important brain functions. These functions included how well they could remember things, how clearly they could think through problems, and particularly how well they could use and understand language. This suggests these pollutants may specifically target and harm these cognitive abilities.
How The Study Was Conducted And Results
To understand this link, the researchers followed a large group of over 1,100 older individuals who were all 65 years of age or older. These seniors were part of a long-running study in Britain that looked at health as people age. The scientists looked at how much air pollution these individuals were exposed to over a period of eight to ten years.
The results of the study showed a clear difference in brain test performance based on where the seniors lived. The older adults who lived in areas that had the highest levels of nitrogen oxide and particle pollution in the air tended to score worse on the tests that measured their brain functions compared to seniors who lived in areas where the air pollution levels were more average. This suggests that living in a more polluted environment can have a noticeable negative effect on cognitive abilities.
Where Do These Pollutants Come From?
The researchers also explained where these harmful pollutants in the air come from. They noted that nitrogen oxide is mainly released into the air when we burn fossil fuels, such as in cars and power plants. On the other hand, fine particle pollution is mostly created by any kind of burning process that releases small bits of ash or soot into the air, like burning wood or from industrial processes. Understanding where these pollutants come from is important for finding ways to reduce them.
The older individuals who lived in the areas with the most polluted air scored in the lowest third on the brain tests that specifically assessed their language abilities. This suggests that the parts of the brain responsible for understanding and using language might be particularly vulnerable to the damaging effects of air pollution compared to other cognitive functions.
This study shows the lasting negative effects of breathing in pollutants on cognitive health in older adults, underscoring the importance of addressing air quality for brain health.
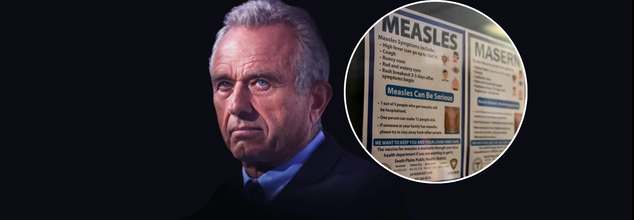
RFK Jr. Urges People To Get Measles Vaccination, 'Didn’t Know’ The Impact Of His Research Cuts
Once considered nearly eradicated in the United States, measles is making a troubling comeback. As of early April, nearly 600 confirmed cases have been reported across multiple states, with Texas emerging as the outbreak’s epicenter. The resurgence of this highly contagious, vaccine-preventable disease is being linked to declining immunization rates, misinformation surrounding vaccines, and weakened public health infrastructure following recent federal budget cuts.
Experts warn that unless aggressive intervention strategies are employed—including increasing vaccination coverage and restoring epidemiological support—the current outbreak could not only persist for months but also jeopardize the U.S.'s measles elimination status achieved in 2000.
In a candid and critical moment of reflection, U.S. Health Secretary Robert F. Kennedy Jr. urged Americans to get vaccinated against measles, even as he admitted on national television that he was unaware of the full impact of significant public health funding cuts enacted during his early tenure. The statement comes amid one of the largest measles outbreaks in recent U.S. history—now spanning multiple states and threatening to reverse decades of progress in infectious disease control.
As of this week, over 595 cases of measles have been confirmed across Texas, New Mexico, Oklahoma, and Kansas. Texas has borne the brunt of the outbreak with 505 cases reported in 21 counties, including urban spillovers that concern local officials. New Mexico has reported 56 cases, Oklahoma 10 (with two still under investigation), and Kansas 24, some of which are believed to be linked to the same source.
The outbreak’s epicenter is Gaines County, Texas—a rural region with low vaccination coverage and limited public health infrastructure. Public health authorities are scrambling to contain the virus, which is known for being highly contagious—transmissible to 90% of unvaccinated individuals in proximity to an infected person.
In his first network television interview since joining President Donald Trump’s cabinet, RFK Jr. sat down with CBS News’ Dr. Jon LaPook for a revealing conversation that quickly became the focus of nationwide scrutiny.
LaPook confronted Kennedy with the administration’s decision to implement $11 billion in cuts to programs targeting infectious diseases, childhood vaccinations, mental health, and addiction support.
“You proposed more than $11 billion in cuts... Did you personally approve those cuts?” asked LaPook.
Kennedy replied, “I’m not familiar with those cuts… Those were mainly DEI cuts, which the president ordered.”
LaPook countered with a specific example, “About $750,000 of a University of Michigan grant into adolescent diabetes was cut. Did you know that?”
“I didn’t know that, and that’s something that we’ll look at,” Kennedy responded, acknowledging that while some reinstatements had occurred, important studies may have been unintentionally defunded due to the sweeping nature of the restructuring.
The CDC’s local partnerships and lab capacities have been severely strained by the budget reductions. Several local health departments, particularly in Texas and New Mexico, have stated that their ability to track, test, and isolate measles cases has been weakened due to the loss of funding and trained personnel.
These challenges are compounded by HHS restructuring, which has resulted in the layoff of more than 10,000 employees under a new directive led by Kennedy in collaboration with the Musk-supported Department of Government Efficiency (DOGE).
“HHS’s job is to make America healthy. We’re spending $1.9 trillion a year and people are not getting healthy,” Kennedy said during the interview. “When you do a disruption of this scale… you may make mistakes in 20% of cases, and then you go back and fix them.”
Yet critics argue that the stakes are too high to risk such large-scale experimental reforms, especially in areas concerning communicable diseases.
Despite his controversial past as a prominent vaccine skeptic, Kennedy used the same interview platform to strongly endorse measles vaccination—a surprising but much-needed pivot.
“We are urging all families in outbreak areas to ensure their children are vaccinated with the MMR vaccine,” Kennedy said, echoing guidance issued by the CDC earlier this week.
The Texas Department of Health Services is now encouraging parents in outbreak zones to get the second MMR dose for children aged 1–4 as soon as possible. Infants between 6–11 months are also eligible for an early dose, with two more to follow on the standard schedule.
The CDC emphasized that 12% of all measles cases this year have required hospitalization, making the situation even more urgent. Experts warn that if the outbreak continues for over 12 months, it could jeopardize the measles elimination status the U.S. achieved in 2000.
The outbreak has cast a spotlight on the fragile state of public health infrastructure, and Kennedy’s remarks have amplified the debate around how to fund and manage it effectively. Though he has promised to revisit specific defunded studies, public health experts remain cautious.
“What we need now is a full restoration of support—not just funds, but trust,” said Dr. Erin Thomas, an infectious disease specialist based in Houston. “These cuts sent a message that infectious disease prevention was no longer a national priority. This outbreak is the direct consequence.”
The statement by the Department of Health and Human Services last week, calling COVID-19 a “non-existent pandemic” and labeling response efforts as wasteful spending, further illustrates the administration’s departure from traditional public health principles.
© 2024 Bennett, Coleman & Company Limited

