Credits: Canva
IVF Nightmare! Woman Gives Birth To A Stranger’s Baby After Embryo Mix-Up
Can you leave your most valued dream—having a baby—into the hands of your fertility clinic? After enduring the emotional, physical, and financial rollercoaster of IVF—only to find out the baby you've carried isn't biologically yours. That's what happened to a woman in Brisbane, Australia, in a case that's now making headlines globally. A Brisbane IVF mix-up has left the world reeling after a woman gave birth to another couple's baby without realizing it, due to a tragic embryo transfer mistake. As this cinematic-style medical disaster unfolds, discussions about embryo safety, fertility ethics, and responsibility are taking center stage.
The incident took place at one of Australia's largest fertility clinics, where a human mistake involved the implantation of a stranger's embryo into another woman by mistake. What happened did not only traumatize the involved families but has raised immediate questions about regulation, ethics, and patient safeguards in the multi-billion-dollar IVF industry.
The error was discovered in February 2025, when the child's biological parents—hereafter called the birth parents—asked for the transfer of their remaining frozen embryos to another fertility clinic. But Monash IVF employees had a shocking discovery: the count of embryos stored was not as recorded. One extra embryo was discovered, giving rise to a chilling finding—one of their embryos had already been implanted in another patient.
Later investigations confirmed that an embryo from this couple had been accidentally thawed and implanted in another woman, who gave birth to a genetically unrelated child.
Monash IVF's CEO Michael Knaap apologized publicly for the incident, referring to it as a moment of profound regret for the organization.
"On behalf of Monash IVF, I would like to express how deeply sorry I am for what has transpired," Knaap stated. "We are distraught, and we apologize to all concerned."
The clinic notified the regulatory bodies, such as the Reproductive Technology Accreditation Committee and Queensland's assisted reproductive technology regulator, and initiated an internal investigation. Knaap reassured the public that extra audits were under way and recalled senior counsel Fiona McLeod to independently examine the breach, committing to adopt all of her findings in full.
Though, this is not the first such scandal Monash IVF has encountered. Earlier this year in 2023, the clinic had agreed on a A$56 million (approx. $36 million USD) class-action lawsuit settlement over claims that up to 700 patients' embryos had been mistakenly destroyed as their genetic screening results had identified these healthy embryos as abnormal.
This case highlights the susceptibility of patients who undergo in vitro fertilization (IVF)—a sophisticated medical procedure where eggs are extracted from a woman's ovaries, fertilized in a laboratory, and inserted into the uterus after they have grown into embryos.
Although IVF brings promise to millions of couples with fertility problems, it's also an emotionally, physically, and financially exhausting process. A single IVF cycle in the U.S. and Australia averages up to $15,000, and success is never assured. Nearly 20,690 babies were born through IVF in Australia and New Zealand in 2021 alone, says the University of New South Wales.
But for all its life-giving possibilities, IVF is impressively procedural, and any leak in protocol—particularly when thawing or transferring embryos—can be irreversible.
Legal, Ethical, and Emotional Consequences of Embryo Mix-up
What is the situation when a woman gives birth to another's child? What are the rights of the biological and gestational parents? These are no longer hypothetical questions—they are now at the center of an existing legal and ethical tempest.
Up to now, Monash IVF has not admitted any liability, although it paid former patients in past accidents. The company maintains this recent mistake was an isolated incident, but critics and lobby groups contend the latest episode indicates systematic failures of quality control and highlights larger issues around transparency within the fertility industry.
The families' identity is protected for legal and psychological reasons, but analysts forecast custody arrangements, emotional trauma, and possible litigation may be the overriding themes in the aftermath for months—if not years—to come.
For a process as precise and delicate as IVF, the value of fail-safe tracking mechanisms, double-checking procedures, and independent reviews cannot be overemphasized. Watchdogs in the U.S., U.K., and other countries are keeping a close eye on the verdict of this case, looking at it as an international warning tale.
In the United States, where IVF is privately funded and unregulated at the federal level, this case may further fuel calls for national oversight boards, improved data transparency, and universal best-practice protocols.
In the meantime, pressure is mounting on advocacy groups to provide psychological counseling for the gestational mother and the biological parents of this traumatic situation. IVF has enabled parenthood for millions. But as technology improves and demand increases, the systems developed to support reproductive health need to improve with similar rigor.
How to Take Psychological Support for Embryo Mix-Ups?
Embryo mix-ups can be emotionally traumatic for all parties involved. Immediate psychological support is crucial to help individuals process shock, grief, and confusion. Offering access to licensed therapists specializing in fertility trauma can create a safe space for emotional expression. Clinics must provide ongoing counseling, not just post-incident, but throughout the legal and ethical aftermath.
Support groups with like individuals can also promote community and empathy. Open communication, compassionate healthcare providers, and trauma-informed care work to restore trust and emotional stability during this very intimate crisis. Prioritizing mental health is crucial for healing.

Credits: Canva
World Liver Day: How A Timely Liver Transplant Saved A 30-Year-Old Man
On World Liver Day, which is observed on April 19, to spread awareness about liver health and the life-saving power of organ donation, let us look at one such real-life story. This is where doctor's prompt's action and one's selfless donation saved one human's life.
When the 30-year-old Delhi-based man walked into the hospital, he had yellow eyes and dangerously high liver enzymes. He was admitted in Max Super Speciality Hospital, Patparganj. That moment, he rarely knew that his life was, in fact, hanging by a thread. The man was diagnosed with acute liver failure, which was caused by viral hepatitis. His body was slowly shutting down. The frequency of his body shutting down had increased. The doctors also quickly informed the family. This was the one last hope of survival - a liver transplant.
The First Option Failed
His sister was family's first ray of hope. She was also willing and had a compatible liver whose part of it could be donated. However, pre-surgery tests revealed that her liver size was too small to ensure a safe transplant. The family then proposed the patient's brother-in-law - a second-degree relative, as the next donor. His liver was a better match, but since he was not an immediate blood relative, there had to be special regulatory approvals which were required.
However, the worsening condition of the patients allowed no such time.
The hospital too scrambled to get clearance for the brother-in-law. All this while, the patient suffered a cardiac arrest. The situation turned dire within minutes. Doctors performed CPR to revive him. He was immediately put on ventilator support. The decision had to be taken soon.
A Miraculous Surgery
With no time in hand, the doctors decided to go ahead with the sister as the donor, though there were risks there too.
A team of highly skilled hepatobiliary surgeons, anesthesiologists, and critical care specialists took over. In a high-risk, nine-hour surgery, they removed the patient’s failing liver and replaced it with part of his sister’s.
“This was one of the most challenging cases we’ve handled,” said Dr. Ajitabh Srivastava, Director – HPB Surgery & Liver Transplant. “When the patient collapsed, our team acted within seconds. Every decision, every move mattered. His survival was truly a team triumph.”
The patient is now recovering well.
What Is A Liver Transplant?
As per the National Institute of Diabetes and Digestive and Kidney Diseases, a liver transplant is a surgical procedure to replace a diseased liver with a healthy one from a donor. It’s often the last resort when liver failure occurs—whether due to chronic illness or sudden injury.
When Is It Needed?
People may need a liver transplant for:
- Alcoholic liver disease
- Fatty liver disease (NASH)
- Cirrhosis due to chronic hepatitis C
- Liver cancer with cirrhosis
- Acute liver failure (often due to drug overdose, hepatitis, or toxins)
Types of Liver Transplants
Deceased Donor Transplant:
The most common type, where a full or partial liver is taken from someone who has recently died.
Living Donor Transplant:
A healthy person donates a portion of their liver—typically a close relative. Both the donor’s and recipient’s liver regenerate to normal size in a few weeks.
What Must Be Kept In The Mind?
- Matching and Compatibility: Blood type, liver size, and health are crucial.
- Approval Process: Especially important for non-blood relatives.
- Recovery and Monitoring: Post-op care involves lifelong medication, lifestyle changes, and regular check-ups.
Rare 100% Deadly Brain Disease Kills Two In Oregon County, Third Infection Confirmed
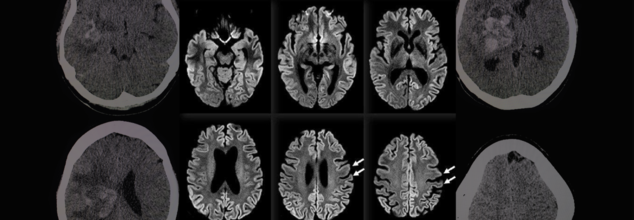
A rare and fatal brain disease with a 100% mortality rate has gripped Hood River County, Oregon, raising concerns within the medical community and eliciting intense probes by local and federal health officials. It is called Creutzfeldt-Jakob Disease (CJD), and it has killed two people and impacted a third in eight months—a terrifying cluster in a county of only slightly more than 23,000 people.
On April 14, the Hood River County Health Department reported one case of Creutzfeldt-Jakob Disease and two more probable cases. Although only one case has been confirmed by a diagnosis through an autopsy, the other two are presumptive and await post-mortem confirmation through examination of brain tissue and cerebrospinal fluid. Such examination, as explained by Trish Elliott, Director of the Hood River County Health Department, may take months.
Although the origins of these three cases are still unknown, the cluster is epidemiologically significant. The U.S. experiences about 350 cases of CJD each year, or 1 to 2 cases per million individuals globally. For Hood River County, with only 23,000 people, to see three cases over such a brief time span is an epidemiologic outlier.
What Is Creutzfeldt-Jakob Disease (CJD)?
Creutzfeldt-Jakob Disease is a rapidly advancing and always lethal neurodegenerative disease resulting from misfolded proteins known as prions. Initially documented in the 1920s by German physicians Hans Gerhard Creutzfeldt and Alfons Jakob, CJD causes sponge-like holes to form within the brain, destroying its structure and function.
CJD is a member of the larger family of prion diseases, which also encompasses other rare but fatal disorders like kuru and fatal familial insomnia. Similar to bovine spongiform encephalopathy (BSE), commonly referred to as mad cow disease, CJD irreversibly destroys the brain and has no cure.
CJD Symptoms and Progression
The symptoms of CJD are extreme and worsen quickly. Early symptoms may involve confusion, disorientation, personality changes, memory loss, visual disturbances, and stiffness of the muscles. Later in the disease, patients can develop hallucinations, difficulty speaking or swallowing, seizures, and sudden jerky movements.
Death typically occurs within a year of the onset of symptoms, usually as a result of complications such as pneumonia, heart failure, or problems arising from neurological deterioration such as falls and choking.
Symptoms in the early stages of sporadic CJD usually resemble other dementias but worsen with terrifying rapidity. The majority of individuals with sporadic CJD are between 50 and 80 years of age, but some genetic forms can occur earlier, even in some people as young as 30.
Various Types of CJD
CJD comes in several types:
Sporadic CJD (sCJD): This type is the most prevalent, affecting about 85% of the cases. This type happens spontaneously when healthy proteins in the brain misfolded into prions for unknown reasons.
Genetic CJD (fCJD): Due to mutations in the PRNP gene, this form is inherited and represents about 10–15% of the total cases. The PRNP gene codes for the prion protein (PrP), a protein involved in neuronal communication and protection.
Acquired CJD (also referred to as iatrogenic or variant CJD): This is a rare type that involves outside sources of infection, such as eating infected beef (BSE/mad cow disease) or through tainted medical equipment or transplanted tissue.
In spite of concerns, authorities from Hood River County stressed that the present cases do not seem to have resulted from infected cows. "At this point in time, there is no cause identified between these three cases," the department noted. They also pointed out that CJD cannot be transmitted via air, touching, social contact, or water.
Public Health Measures and Continued Investigations
The Hood River County Health Department, in collaboration with the Oregon Health Authority and the Centers for Disease Control and Prevention (CDC), has launched an "active and ongoing investigation" into the three reported cases.
“We’re trying to look at any common risk factors that might link these cases,” Trish Elliott told The Oregonian. “But it’s pretty hard in some cases to come up with what the real cause is.”
Although risk to the general population is "extremely low," the health department continues to monitor it. Since CJD cannot be definitely diagnosed until after death, real-time monitoring is not easy, and so robust surveillance is essential.
Can CJD Be Prevented?
Although there is no treatment or cure to prevent the development of CJD, the U.S. has established strict public health measures to minimize the risk of acquired CJD, especially through food supply control and medical safety measures.
Federal authorities have maintained since the 1990s a prohibition against feeding cattle which could be contaminated with BSE, and employment of high-risk material in foods is strictly barred. Sterilization processes of surgical devices as well as strict donor screening in transplantation and transfusions are all undertaken to cut back on iatrogenic spread.
While medical officials wait for further verification and possible connections between the three patients, the attention is on education, surveillance, and reassurance to the public.
Although it is reassuringly ominous to witness a disease of this kind emerging in a small American community, the risk at the international level remains low, especially with measures presently in place. Nevertheless, the cases are a sobering reminder of the enigma that prion diseases continue to pose to modern medicine.
Health officials are still keeping an eye on the matter and are asking people not to panic but to remain updated. "The health department will remain vigilant and inform you of any public health risk," officials promised in a statement.

Credits: Canva
Medical Cannabis May Help Fight Cancer, Largest-Ever Study Shows Potential To Treat Symptoms
The largest-ever scientific study on cannabis and cancer has shown strong evidence that medical cannabis can do more than treat symptoms — it could actually fight the disease itself. The research, published in Frontiers in Oncology, provides a robust and data-heavy analysis that brings much-needed clarity to a very contentious issue.
Led by Ryan Castle, Research Director of the Whole Health Oncology Institute, this revolutionary analysis converges more than 10,000 studies — the largest such inquiry into medical cannabis and cancer to date.
Cannabis has been in the middle of medical controversies and legislative wars for a long time. Traditionally, the Schedule I status of cannabis under federal law has limited high-quality human clinical studies, preventing the medical community from reaching a consensus. Castle and his colleagues aimed to change that.
Our aim was to establish the scientific consensus on the issue of medical cannabis, an area that has been long dominated by a war of cherrypicked studies," Castle said.
In order to transcend prejudice, Castle's team took the large-scale, inclusive approach fuelled by AI and sentiment analysis — a process widely employed by natural language processing to determine whether written material portrays a positive, neutral, or negative sentiment. Here, AI analyzed thousands of abstracts and conclusions drawn in scientific literature to determine whether each one stated agreement, neutrality, or doubt in cannabis's applicability to the treatment of cancer and symptom alleviation.
The result? An overwhelming majority of studies presented a positive view, indicating medical cannabis holds therapeutic value not just for symptom relief — such as reducing inflammation and nausea or boosting appetite — but potentially for accelerating apoptosis, the death of cancer cells.
Castle's group examined over 10 times the amount of research examined in any other meta-analysis. Their report stated that roughly 55% of studies indicated a positive relationship between medical cannabis and favorable cancer outcomes with only a few percent reporting adverse effects or none at all.
That percentage — 55% — may seem humble, but with the sheer scale of the data and the scientific conservative tradition in this area, it's telling. "This level of statistical consensus is precisely what we required to start thinking of cannabis as more than an edgy cure-all," Castle wrote.
In addition, the National Cancer Institute (NCI) revealed that 20% to 40% of patients with cancer currently use marijuana products to deal with side effects such as constant pain, chemotherapy-related nausea and vomiting, and sleeplessness. Still, investigations had fallen behind trend usage rates based on government policy and availability of funds in the past.
It is valuable to place the results of this mega-study in the context of the overall body of cannabis research. Much of what is published is derived from in vitro (test tube) experiments or animal models and not human trials. However, several of these studies have promising results: compounds found in cannabis — particularly cannabinoids such as delta-9 THC, CBD, and CBG — have been shown to inhibit cancer growth, prevent metastasis, and cause cancer cell death in laboratory experiments.
A 2023 Discover Oncology study supported this perspective, reaching the conclusion that multiple cannabinoids reveal "promising potential as anticancer agents by multiple mechanisms." These include curbing tumor expansion, inhibiting cancer cell invasion, and cutting inflammation — which is a documented driver of cancer growth.
In addition, more recent studies have discovered unforeseen advantages in cancer patients who use cannabis. A University of Colorado study reported that patients who consumed marijuana products from licensed dispensaries for a two-week period reported better thinking and cognition, contrary to previous concerns that cannabis would impair mental sharpness in chronic users.
Even with all the encouraging results, Castle and other specialists advise not to consider cannabis a panacea. The available evidence does not indicate that medical cannabis by itself can heal cancer. Rather, its actual strength is in integrative oncology — as an adjunct therapy in addition to standard therapies such as chemotherapy, radiation, and immunotherapy.
This is in agreement with results of a 2019 literature review, which noted that cannabis potentially slows cancer growth and aids improved treatment outcomes, although its effectiveness is highly variable based on cancer type, formulation of cannabinoids, and dose.
One of the significant challenges that persist in holding back development in this arena is the federal classification of cannabis as a Schedule I drug. According to existing U.S. policy, cannabis is listed alongside drugs such as heroin — a designation that presents many legal and bureaucratic hurdles to researchers and healthcare professionals.
In addition, in the Trump era, the National Cancer Institute highlighted marijuana as one of almost two dozen "controversial or high-profile issues" that needed extra clearance prior to publication or research sharing. This culture of fear and repression has only held back the much-needed research into medical cannabis's complete potential.
The biggest-ever analysis of medical cannabis and cancer isn't asserting to have discovered a cure but what they have discovered is a mounting scientific concurrence that medical cannabis should be included in mainstream discussions of cancer treatment. From reducing side effects to having the potential to interfere with cancer cell life cycles, cannabis might have more than just palliation to provide — it might have clinical benefit.
© 2024 Bennett, Coleman & Company Limited

