
Credits: Canva
India Bans Cough Syrups For Children Under 4 Due To Safety Concerns
In a breakthrough step towards safeguarding infant and toddler health, the Government of India has formally prohibited the use of some commonly found over-the-counter (OTC) cough and cold medicines in children below the age of four. This policy move, as notified by the Union Ministry of Health and Family Welfare through a gazette notification, prohibits the use of a fixed-dose combination (FDC) of Chlorpheniramine Maleate and Phenylephrine Hydrochloride—two ingredients found in many pediatric cough syrups.
The decision follows an increasingly vocal global health chorus of alarm at the safety of these products among very young children, India now being among the latest to make strong regulatory moves.
The fixed-dose combination in question has been used to alleviate symptoms of the common cold and allergic rhinitis for a long time. Nonetheless, after reviewing the same, a Subject Expert Committee (SEC) constituted by the Central Government with suggestions from the Drugs Technical Advisory Board (DTAB) opined that this combination is likely to produce risks for children under four years of age—risks overweighing possible benefits.
As per the Health Ministry's statement, "the use of the fixed-dose combination is likely to pose risk to children under the age of four, and safer options to the aforementioned drug are in place."
The government used Section 26A of the Drugs and Cosmetics Act, 1940, to limit the production, sale, and supply of these formulations for pediatric administration in India.
What Are These Drugs?
The now-restricted combination consists of two commonly prescribed ingredients:
Chlorpheniramine Maleate: An antihistamine that operates by inhibiting histamine receptors in the body, relieving symptoms such as sneezing, watery eyes, and runny nose.
Phenylephrine Hydrochloride: A decongestant that constricts blood vessels in the nostrils to narrow them and improve breathing.
Collectively, they've had different brand names and are household essentials in all Indian homes for treating cold as well as allergy conditions. The preparations, though usually safe for adults and older kids, are found to be potentially unsafe for toddlers.
Why the Risk is Greater for Toddler?
Infants under the age of four are at greater risk for side effects due to their immature organ systems and lower body weight. Even normal doses can produce exaggerated physiological effects.
Drowsiness, restlessness, dizziness, or even paradoxical excitation (hyperactivity rather than sedation) can result from chlorpheniramine and be particularly hazardous in infants.
Phenylephrine is a stimulant that can raise blood pressure, induce palpitations, and produce headaches. Its vasoconstricting effect, while useful in nasal decongestion, can impose excessive strain on a child's cardiovascular system.
All these compounds, when used in combination, have an intricate pharmacological profile that can do unintended damage if taken without tight medical surveillance.
Apart from prohibiting the mixture for children under four, the government has asked manufacturers to put a clear warning label on all packaging, inserts, and advertising materials.
The warning that must be used is: This fixed-dose combination shall not be used in children below four years of age.
This choice isn't just a one based on regulation but rather an educational choice as well, trying to notify parents, caregivers, and healthcare workers of the danger of self-medicating infants and toddlers outside of a physician's recommendation.
Are There Safer Alternatives?
Yes, the prohibition is the result of the availability of safer, more targeted alternatives. Pediatricians frequently suggest utilizing saline nasal drops, humidifiers, or warm liquids to relieve cold symptoms in children. In more severe instances, medications targeting specific symptoms are prescribed under close dosage control.
It's crucial to keep in mind that a majority of colds are viral infections that naturally go away by themselves. Medicating symptoms with aggressive medication, particularly in kids under four years old, more often than not causes more damage than good.
What Should Parents Do Now?
- Talk to pediatricians before administering any OTC cold or allergy medication to kids.
- Don't use leftover or adult-strength formulas, even in reduced amounts.
- Read labels before buying drugs and look for the new government-required warning.
- Watch for side effects if the drug has already been taken and obtain instant medical care for any side effects.
India's regulatory action reflects worldwide thinking. Other nations such as the U.S., Canada, and the U.K. had earlier issued guidelines or warnings concerning the use of OTC cough and cold medicines among young children.
In the United States, the FDA recommends against administration of cold drugs to children less than two and cautions against even those two to six. Likewise, the American Academy of Pediatrics (AAP) has cautioned against the use of OTC cough and cold medicines in kids less than four years old as a matter of long-standing concern regarding insufficient benefit and possible risks.
India's move is consistent with this evidence-based strategy, reinforcing the global push toward child-specific formulations, careful monitoring, and public health education.
The prohibition on children under four using cough syrup combinations is an important step towards more rational and safer use of drugs in pediatric care. As greater awareness emerges regarding the subtleties of treating younger children, particularly in non-clinical environments, policy like this one serves to protect the most vulnerable groups.
For parents, the message is simple: drugs that are effective for adults or older kids are not necessarily safe for toddlers. If it's questionable, always call a physician.

Credit: Canva
UK Recalls Common Blood Pressure Drug Over Packaging Error
Patients taking a widely used blood pressure drug are being advised to verify their medication after a batch was recalled due to incorrect dosage information printed on the packaging. According to the Medicines and Healthcare Products Regulatory Agency (MHRA), some packs of lercanidipine, manufactured by Recordati Pharmaceuticals, have been wrongly labelled as containing 10mg tablets, when in fact they contain 20mg tablets.
Over 7000 Packs Are Subject To Recall
More than 7,700 packs already distributed are now subject to the recall, the MHRA has confirmed. Patients who may have the mislabelled medication are being urged to contact their GP, pharmacist, or call NHS 111 for advice. The NHS warns that consuming an excessive dose of lercanidipine can lead to symptoms such as dizziness and drowsiness. The MHRA issued the alert on Thursday after being informed by the Italian pharmaceutical company Recordati that the error was confined to a single batch of lercanidipine, which was initially distributed on April 10. The recalled packs carry the batch number MD4L07 and are marked with an expiry date of January 2028.
Although the front of the affected packs displays the incorrect strength, the correct 20mg dose is printed on the blister strips inside and on the side of some of the boxes. The MHRA advises patients who have been prescribed the 20mg dose to check the blister packaging to ensure they have received the correct medication. However, those prescribed 10mg tablets should seek immediate medical attention if they have this batch.
As a temporary measure, the MHRA suggests that patients who cannot reach a healthcare provider may take half of a 20mg tablet until they receive professional guidance. Dr Alison Cave, the MHRA’s chief safety officer, stated: "Healthcare professionals such as pharmacists are also being asked to stop supplying medicine from the affected batch and to return it to the supplier." She encouraged anyone experiencing suspected side effects to report them through the MHRA’s Yellow Card scheme.
In a statement to the BBC, a spokesperson for Recordati said the company is "working proactively" with the MHRA and will contact all customers who might have received the affected batch. “We are investigating the root cause and continue to work with our partners to isolate the issue and minimise disruption to our patients. Patient safety remains our top priority,” the spokesperson added.
What Do We Know About Lercanidipine?
Lercanidipine is used in the treatment of Angina (heart-related chest pain), Hypertension (high blood pressure), Arrhythmia, hypertensive emergency, subarachnoid haemorrhage and anal fissure. According to the NHS, it is one of the four types of blood pressure medicines sold across the UK. These pills are a calcium channel blocker. That means it regulates blood pressure by relaxing blood vessels and reducing pressure on them, thereby making it easier for the heart to pump more blood throughout the body. In this way, it normalises the blood pressure in patients with high blood pressure.
ALSO READ: RFK Jr.'s Autism Controversial Comments Face Backlash From Parents And Medical Experts
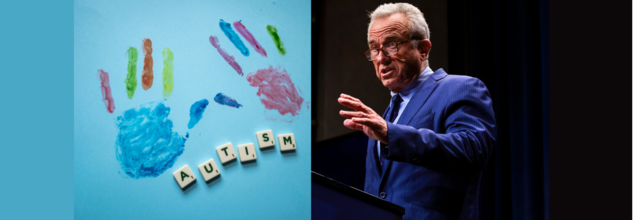
RFK Jr.'s Autism Controversial Comments Face Backlash From Parents And Medical Experts
Robert F. Kennedy Jr., the U.S. Secretary of Health and Human Services, is facing strong backlash after making sweeping comments during a recent press conference regarding autism and its supposed causes. As the CDC released a report revealing a rise in autism diagnoses among U.S. children now affecting 1 in 31 8-year-olds Kennedy doubled down on discredited theories linking autism to environmental exposures and vaccines, while portraying the disorder in stark, stigmatizing terms.
His remarks including claims that children with autism “will never hold a job,” “never pay taxes,” or “never use a toilet unassisted”, were swiftly condemned by parents, medical experts, and advocacy groups alike for reinforcing outdated stereotypes and misrepresenting the broad and diverse autism spectrum.
Autism spectrum disorder (ASD) is not a single condition with uniform symptoms or outcomes. Rather, it is a neurological and developmental condition characterized by challenges in social interaction, communication, and repetitive behaviors. The key word is "spectrum" and it exists for a reason.
Some individuals with autism may be nonverbal and need lifelong support, while others live independently, excel in careers, write books, or even hold public office. “Autism is not a disease,” said actress and autism advocate Holly Robinson Peete in a video statement, responding to Kennedy. “It is a developmental difference and it is important to get that right.”
Her son, RJ, diagnosed 25 years ago, has “shattered a lot of 'never' off that list,” she said, referring to Kennedy’s grim portrayal. Countless parents echoed this sentiment on social media, stating that Kennedy’s generalizations erase the lived realities, milestones, and accomplishments of their children.
CDC Data Shows a Rise in Diagnoses
The CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network reported that 1 in 31 8-year-olds in the U.S. were diagnosed with autism in 2022, compared to 1 in 54 in 2016. But experts stress that this increase is not necessarily cause for alarm. It is, in fact, a sign of progress.
The rise in autism rates is driven largely by improved awareness, broader diagnostic criteria, and increased access to evaluations and services. We are identifying children earlier and more accurately that’s a good thing.
Kennedy, however, rejected this explanation as “indefensible” and announced plans for a directive to the National Institutes of Health to investigate “environmental exposures” as the root cause — reigniting long-debunked concerns about vaccines and toxins.
Despite overwhelming scientific consensus debunking any link between vaccines and autism, Kennedy has long been associated with promoting vaccine hesitancy. His latest comments, veiled in language about “environmental exposures,” once again hint at this discredited narrative.
Leading medical organizations, including the American Academy of Pediatrics and the World Health Organization, have repeatedly emphasized that vaccines are safe, effective, and have no causal relationship with autism. Resurrecting these claims only spreads fear and confusion. It undermines public health and harms autistic people by framing their existence as a preventable tragedy.
Parents Demand a Shift in the Narrative
Perhaps the strongest rebuke came from parents of autistic children themselves. Samantha Taylor, whose 20-year-old son is on the spectrum, told Good Morning America, “Autism doesn’t destroy families misinformation does.” In a viral Facebook post, she added, “What truly causes damage is the relentless portrayal of autism as something catastrophic, rather than a different way of experiencing the world.”
Kennedy’s comments, they say, not only ignore the complexity of the condition but strip children of their dignity and potential.
“Statements like ‘they’ll never write a poem’ deny the creative genius that so many autistic individuals demonstrate,” said Peete. “It’s dangerous, it’s harmful, and it’s simply false.”
Experts Call for More Informed Leadership
While Kennedy has promised answers by September through federally backed studies, medical experts warn that his rhetoric may set back years of advocacy and research by framing autism as an “epidemic” akin to an infectious disease.
Autism is not something to be eradicated, it’s something to be understood, supported, and embraced. Families deserve resources, not fearmongering.
In the last two decades, the medical community has shifted toward neurodiversity — a perspective that recognizes neurological differences like autism as natural variations of the human genome. This philosophy emphasizes inclusivity, respect, and strength-based approaches rather than medicalizing difference.
At a time when public trust in institutions is fragile, the words of public officials matter deeply. Kennedy’s comments have triggered a reckoning not only about how autism is portrayed in the media and politics but also about how society chooses to value — or devalue — people who are different.
Advocates stress the need for policies rooted in science, not stigma, and for leadership that uplifts rather than marginalizes.
As the national conversation around autism continues, one thing is clear: the autism community — parents, children, adults on the spectrum, clinicians, and allies — is not going to stay silent in the face of outdated narratives.

Credits: Canva
World Liver Day: How A Timely Liver Transplant Saved A 30-Year-Old Man
On World Liver Day, which is observed on April 19, to spread awareness about liver health and the life-saving power of organ donation, let us look at one such real-life story. This is where doctor's prompt's action and one's selfless donation saved one human's life.
When the 30-year-old Delhi-based man walked into the hospital, he had yellow eyes and dangerously high liver enzymes. He was admitted in Max Super Speciality Hospital, Patparganj. That moment, he rarely knew that his life was, in fact, hanging by a thread. The man was diagnosed with acute liver failure, which was caused by viral hepatitis. His body was slowly shutting down. The frequency of his body shutting down had increased. The doctors also quickly informed the family. This was the one last hope of survival - a liver transplant.
The First Option Failed
His sister was family's first ray of hope. She was also willing and had a compatible liver whose part of it could be donated. However, pre-surgery tests revealed that her liver size was too small to ensure a safe transplant. The family then proposed the patient's brother-in-law - a second-degree relative, as the next donor. His liver was a better match, but since he was not an immediate blood relative, there had to be special regulatory approvals which were required.
However, the worsening condition of the patients allowed no such time.
The hospital too scrambled to get clearance for the brother-in-law. All this while, the patient suffered a cardiac arrest. The situation turned dire within minutes. Doctors performed CPR to revive him. He was immediately put on ventilator support. The decision had to be taken soon.
A Miraculous Surgery
With no time in hand, the doctors decided to go ahead with the sister as the donor, though there were risks there too.
A team of highly skilled hepatobiliary surgeons, anesthesiologists, and critical care specialists took over. In a high-risk, nine-hour surgery, they removed the patient’s failing liver and replaced it with part of his sister’s.
“This was one of the most challenging cases we’ve handled,” said Dr. Ajitabh Srivastava, Director – HPB Surgery & Liver Transplant. “When the patient collapsed, our team acted within seconds. Every decision, every move mattered. His survival was truly a team triumph.”
The patient is now recovering well.
What Is A Liver Transplant?
As per the National Institute of Diabetes and Digestive and Kidney Diseases, a liver transplant is a surgical procedure to replace a diseased liver with a healthy one from a donor. It’s often the last resort when liver failure occurs—whether due to chronic illness or sudden injury.
When Is It Needed?
People may need a liver transplant for:
- Alcoholic liver disease
- Fatty liver disease (NASH)
- Cirrhosis due to chronic hepatitis C
- Liver cancer with cirrhosis
- Acute liver failure (often due to drug overdose, hepatitis, or toxins)
Types of Liver Transplants
Deceased Donor Transplant:
The most common type, where a full or partial liver is taken from someone who has recently died.
Living Donor Transplant:
A healthy person donates a portion of their liver—typically a close relative. Both the donor’s and recipient’s liver regenerate to normal size in a few weeks.
What Must Be Kept In The Mind?
- Matching and Compatibility: Blood type, liver size, and health are crucial.
- Approval Process: Especially important for non-blood relatives.
- Recovery and Monitoring: Post-op care involves lifelong medication, lifestyle changes, and regular check-ups.
© 2024 Bennett, Coleman & Company Limited

