
FDA Gives A Green Light To Blujepa For Treating Uncomplicated UTIs
Among the many latest approvals, the US Food and Drug Administration (FDA) has approved Blujepa (gepotidacin) for the treatment of uncomplicated urinary tract infections (uUTIs) in adult women who weigh 40 kg or more and for children who are 12 years and older and weigh 40 kg or more.
What Is Blujepa?
It is a first-in-class oral antibiotic which is approved for the treatment of uUTIs which are caused by Escherichia coli, Klebsiella pneumoniae, Citrobacter freundii complex, Staphylococcus saprophyticus, and Enterococcus faecalis.
How Was It Approved?
The approval followed the results form the Phase 3 EAGLE-2 and EAGLE-3 trials. These trials were useful to demonstrate the medication's noninferiority and superiority, respectively, to nitrofurantoin, which is one of the leading current standard-of-care options available for uUTIs in women and pediatric patients. This is for patients with confirmed uUTI.
What were the results of these trials?
In EAGLE-2, the therapeutic success occurred in 50.6 percent of patients taking Blujepa compared with 47.0 percent of those taking nitrofurantoin. In EAGLE-3, the superiority was demonstrated for Blujepa versus nitrofurantoin, with therapeutic success occurring in 58.5 versus 43.6%.
Are there any side effects of Blujepa?
One of the most common adverse events that patients who have consumed Blujepa reported was gastrointestinal, including diarrhea, which was reported in 16% of the patients. Then came nausea at 9%.
The maximum severity of these side effects or adverse events were mostly mild up to 69% to moderate at 28%. Severe gastrointestinal events occurred only in less than 1% of all the participants.
"The approval of Blujepa is a crucial milestone, with uUTIs among the most common infections in women," Tony Wood, chief scientific officer of GSK, said in a statement. "We are proud to have developed Blujepa, the first in a new class of oral antibiotics for uUTIs in nearly three decades, and to bring another option to patients given recurrent infections and rising rates of resistance to existing treatments."
What Is Uncomplicated UTI?
As per the National Library of Medicine's National Center for Biotechnology Information, an uncomplicated UTI is a bacterial infection of the bladder and associated structures. Patients with uUTI have no structural abnormality of the urinary tract and no comorbidities such as diabetes, an immunocompromised state, recent urologic surgery, or pregnancy. A uUTI is also known as cystitis or lower tract UTI.
The presence of bacteria (bacteriuria) or white blood cells (pyuria) in the urine without symptoms does not indicate a urinary tract infection (UTI). Common UTI symptoms include frequent urination, urgency, suprapubic discomfort, and pain during urination (dysuria). While UTIs are common in women, they are rare in circumcised males. When they do occur in circumcised males, they are typically classified as complicated UTIs.
Many uncomplicated UTIs can resolve on their own, but treatment is often sought to relieve symptoms and prevent the infection from spreading to the kidneys. If left untreated, a UTI can develop into an upper tract infection like pyelonephritis, which can damage kidney structures and potentially lead to high blood pressure.
A UTI diagnosis is based on clinical history and urinalysis, with confirmation through a urine culture. Proper urine sample collection is crucial for accurate evaluation and diagnosis.

Credits: Canva
These 24 Pathogens Could Trigger The Next Pandemic, Says UKHSA
Pathogens are responsible for diseases like bird flu, COVID-19, and bat-borne viruses that cause brain swelling. They pose a serious risk to public health, according to biosecurity experts in the United Kingdom. The UK Health Security Agency (UKHSA) has recently identified 24 pathogen families that require urgent attention due to their potential to cause outbreaks and pandemics.
Why These Pathogens Are A Concern?
The UKHSA has categorized these pathogens as threats for several reasons:
High Contagion and Severe Disease: Some pathogens spread rapidly and cause serious illness, increasing their risk of global outbreaks.
Lack of Vaccines and Treatments: Many of these diseases do not have effective vaccines or treatments, making containment difficult.
Impact of Climate Change: Rising temperatures and environmental shifts may enable the spread of diseases to new regions.
Antibiotic Resistance: Some pathogens are evolving resistance to available treatments, making infections harder to manage.
Which Pathogens Have Made It To The List?
- Mpox (formerly monkeypox)
- Coronaviruses (including COVID-19)
- Norovirus (winter vomiting bug)
- Influenza (including avian flu)
- Gonorrhoea (due to antibiotic resistance)
- Ebola and Zika viruses
- Lassa fever and Nipah virus (both capable of causing severe illness and outbreaks)
High-Risk Pathogens with Pandemic Potential
Eight of the identified pathogen families have been categorized as high or medium risk for triggering a pandemic. While some have vaccines and treatments in development, many remain in clinical trial stages, leaving the world vulnerable to future outbreaks.
UKHSA experts emphasized the need for further research and investment to prevent these pathogens from escalating into major health crises.
The Importance of Research and Investment
Dr. Isabel Oliver, UKHSA’s Chief Scientific Officer, stated that this identification process is crucial for directing resources where they are most needed. “We hope this will help to speed up vaccine and diagnostics development where it is most needed, to ensure we are fully prepared in our fight against potentially deadly pathogens,” she said.
The Debate Over the Pathogen List
Independent experts have acknowledged the usefulness of the UKHSA list in focusing research and preparedness efforts. However, concerns remain about the exclusion of other potential threats.
Jose Vazquez-Boland, an infectious disease expert at the University of Edinburgh, warned that prioritizing certain pathogens could divert attention and funding from other dangerous but overlooked diseases.
Emma Thomson, Director of the MRC-University of Glasgow Centre for Virus Research, stressed the importance of regularly updating the priority list. “It is essential that this list remains dynamic and responsive to emerging threats,” she said. History has shown that pandemics can arise from unexpected sources.
Climate Change and the Spread of Disease
Dr. Oliver also highlighted the increasing risk posed by climate change, particularly in the spread of vector-borne diseases. Changing temperatures and shifting ecosystems are altering the distribution of mosquitoes and ticks, which carry diseases such as dengue and Zika.
Lessons from the COVID-19 Pandemic
A report from the UK COVID-19 inquiry found that prior to 2020, pandemic preparedness focused too much on influenza, leading to delays in responding to COVID-19. Experts now emphasize the need to prepare for a wide range of threats, including unknown “Disease X” pathogens.
Mark Woolhouse, an epidemiologist at the University of Edinburgh, warned that a novel measles-like virus could pose an even greater threat than COVID-19. “Such a virus would be more contagious than the original COVID-19 variants, impossible to control with lockdowns, and more deadly—especially to children,” he said.

Credits: Canva
Utah Becomes The First State To Ban Fluoride In Water
Utah has become the first state to ban fluoride in public drinking water. This has been opposed by dentists and national health organizations who had warned that this move could lead to more medical problems, dental problems and could also disproportionately affect low-income communities.
Spencer Cox, Republican Gov. signed the legislation on Thursday that barred cities and communities from deciding whether to add the mineral to their water systems.
What Does Fluoride Do?
Fluoride strengthens teeth and reduces cavities by replacing minerals lost during normal wear and tea. The US Centers for Disease Control and Prevention (CDC) notes that they are naturally occurring compounds and when used in low levels, it can help prevent dental cavities.
The CDC notes that fluoride repairs and prevents damage to teeth caused by bacteria in the mouth. Bacteria in the mouth produce acid when a person eats or drinks. The acid then dissolves minerals in a tooth’s surface and makes the tooth weaker and open to cavities.
Fluoride also replaces the minerals lost from a tooth due to acid breakdown. Some fluoride can replace minerals in the tooth surface, which makes the outer enamel layer harder to dissolve. Fluoride also could reduce the amount of acid that cavity-causing bacteria produce, as well as making it harder for these bacteria to stick to the teeth.
CDC notes that teeth requires consistent, low levels of fluoride in the mouth, in the saliva and on tooth surfaces. Fluoride can also be incorporated into developing dental enamel before a tooth erupts into the mouth, enhancing the tooth’s resistance to acid breakdown and preventing cavities later in life.
As per the US Food and Drug Administration, the fluoride levels in the water is regulated and are safe and effective when used as directed. However, despite this, Utah has banned its use.
ALSO READ: Utah To Become The First State To Ban Fluoride In Drinking Water
What Happened In Utah, Why The Ban?
Utah lawmakers pushed for fluoride ban stating that it was too expensive. As per Cox, he grew up and raised his own children in a community without fluoridated water. The ban will be effective from May 7. This move has been promoted by the US Health Secretary Robert F Kennedy Jr, who expressed skepticism about water fluoridation.
As per the American Dental Association, this is a move worth criticizing. They said that the ban showed “wanton disregard for the oral health and well-being of their constituents.” The group said that cavities are the most common chronic childhood disease.
“As a father and a dentist, it is disheartening to see that a proven, public health policy, which exists for the greater good of an entire community’s oral health, has been dismantled based on distorted pseudoscience,” said the association’s president, Denver dentist Brett Kessler, as reported by the CNN.
In elsewhere too, including Ohio, South Carolina, and Florida, similar proposals have been made to restrict local governments or water system operators from adding fluoride to water. Whereas such proposed restrictions have been rejected in New Hampshire, Tennessee and North Dakota.
Credits: Instagram & Canva
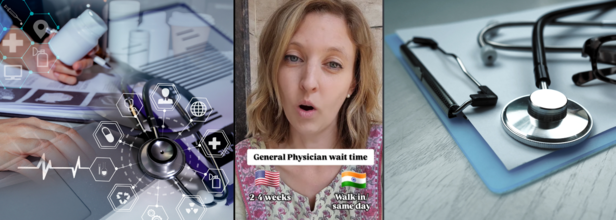
American Woman Who Compared US Healthcare System With India Says Affordability Is An Issue In America
Kristen Fischer, an American woman living in India who works in web development sparked a new debate. This is between the healthcare systems of two big countries, the United States and India. The woman took to her Instagram @kristenfischer3 with 143K followers and shared a video titled 'Healthcare in India and the USA'. The video garnered over 51.6K views and with many more interactions.
Her video starts with comparing the wait time of a GP. In the US, the average wait time, she mentions is 2 to 4 weeks, whereas in India, it is a walk-in or same-day appointment. She mentions in the caption that in India, healthcare is more accessible and there is an easy to access doctors, medicines, and quality care. She also talks about how easily medicines are accessible in India and over-the-counter medicines could be picked without a prescription.
What Really Are The Big Differences In Healthcare Between The Two Countries?
Wait Time
One of the biggest differences that Kristen highlights is of the wait time for medical consultation. In the US, scheduling an appointment with a GP can lead to even a month of wait time. It can further extend to three months. For elective surgeries or planned and non-emergency surgeries, the wait time could be for as long as six months.
Whereas, if one looks at India, the access is faster. There are appointments, which can be booked within a few days, furthermore, walk-in services are also available in most cases. Elective surgeries are usually performed within one to four weeks in India.
Cost Of Medical Consultation
Healthcare in the US is costly. Kristen writes in her caption: "In America, we hardly went to the doctor because it was just so expensive and you had to wait weeks to get in. But I have peace of mind in India knowing that I can go to a doctor any day even for something small because it is affordable.”
It is true, on an average, for a visit to a doctor in America could cost anyone between $150 to $600, which is around 12k to 50k INR. Whereas in India, the consultation cost is between $7 to $17, which could be around 500 to 1,500 INR. The affordability is what ensures that people do not hesitate to reach out to doctors or healthcare professionals when in need.
Hospitalization Expense
Not just appointments with doctors, but in the US, the hospitalization costs are also skyrocketing. For one-night hospital stay, the cost is around $3,000, which is somewhere around 2.5 lakhs INR. This makes hospitalisation a financial burden, even for those under insurance.
In India, one day stay at a hospital is around $80, which could be around 6,000 INR.
Medical Insurance
There are also arguments that the US healthcare system is manageable as it is covered in medical insurance. However, the reality may be different, because the medical insurance too is not quite affordable. The average cost of medical insurance in the US could range somewhere between $800 and $1,500, which could be around 64k to 1.2 lakh INR per month. There are also high premiums.
Whereas in India, the medical insurance is far for affordable, ranging between $23 and $58, around 2k to 5k INR.
Quality of healthcare services
While the US is home to the best medical facilities, world-class research and top-tier doctors, it does come at a very high price. However, the Indian healthcare system is a mix of both, private and public hospitals, where experts come from all walks of life. In fact, at this time, many private hospitals too have been technologically equipped and have internationally accredited doctors.
The biggest point to be noted, as Kristen also mentions, is the affordability the Indian healthcare system offers and the understanding of treating medical cases with urgency.
© 2024 Bennett, Coleman & Company Limited

