- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can Weight Loss Drugs Curb Alcoholism? See What Study Says

Credits: Canva
Until law, GLP-1 drugs were used to treat diabetes, obesity and even the recent evidences suggest that it could as well be used to treat chronic kidney problems. There is yet another research, published in JAMA Psychiatry on February 25, titled Once-Weekly Semaglutide in Adults With Alcohol Use Disorder: A Randomized Clinical Trial that explores if GLP-1 receptor agonist semaglutide reduce alcohol consumption and cravings in adults with alcohol use disorder.
What Do Studies Say?
The research was conducted over a period of 9 weeks, where in the randomized clinical trial, the participants who were administered semaglutide, it led to reductions in some but not all measures of weekly consumptions. It also reduced weekly alcohol and craving related to placebo, and also led to a greater relative reduction in cigarettes per day.
The research also found that weekly injections of semaglutide, which is the active ingredient in weight loss drugs like Wegovy also helped reduce cravings in people with alcohol use disorder.
The lead author Christian Hendershot said that these findings will help in developing new approaches to treat alcoholism. "Two drugs currently approved to reduce alcohol consumption aren't widely used. The popularity of Ozempic and other GLP-1 receptor agonists increases the chances of broad adoption of these treatments for alcohol use disorder," said Hendershot in news release by the University of Southern California's Institute for Addiction Research, where he is the director.
The study is government-funded research and was funded by the National Institute on Alcohol Abuse and Alcoholism, part of the National Institutes of Health.
How Was The Study Conducted?
The study was small, and took in account for only 48 adults over two months, thus experts say that it is not yet clear how safe these drugs are for people who do not need to lose weight. Though the results do add up with the evidence form animal studies on drugs like Ozempic and Wegovy on how it helps manage cravings, not just for food, but also for tobacco and alcohol. Scientists are also studying these drugs on smokers, people with opioid addiction and cocaine users.
Co-author Dr Klara Klein of the University of North Carolina at Chapel Hill who treats people with obesity and diabetes said, "This is such promising data. And we need more of it. We frequently will hear that once people start these medications that their desire to drink is very reduced, if not completely abolished."
Why Does It Work So Well Against Alcoholism?
The GLP-1 receptor agonists work by mimicking hormones GLP-1 in the gut and brain that regulates appetite and feelings of fullness. This response is what helps one lose weight, and what helps one curb their craving for alcohol. These drugs that mimic the functioning of your brain, which is responsible to tell your body when to stop consuming, are the same hormones that tell your body about other kinds of consumptions, including alcohol. Therefore by consuming the weight loss drugs one can treat alcohol use disorder.
However, the researchers have pointed out on the limited data on the research and have suggested to continue using the three approved drugs by the National Institute on Alcohol Abuse and Alcoholism and Substance Abuse and Mental Health Services Administration, namely, Disulfiram, Naltrexone, and Acamprosate to treat alcohol use disorder until large studies confirm these findings.
Travel Vaccine Update: CDC Issues Travel Advisory Against 32 Countries For Poliovirus

Credits: Canva
On March 9, the United States issues a travel advisory against global polio and listed 32 countries, including some European countries. The International travel often comes with vaccine reminder and health checks to stay safe. The Centers for Disease Control and Prevention (CDC) issued a Level 2 travel advisory for certain international destinations with circulating poliovirus. The CDC has asked travelers to ensure they are up to date on their polio vaccines.
Also Read: Harish Rana Case Brings Spotlight On How Passive Euthanasia Has Evolved Over The Years
The Destination list for global polio travel Advisory notice includes:
- Afghanistan
- Algeria
- Angola
- Benin
- Burkina Faso
- Cameroon
- Central African Republic
- Chad
- Côte d'Ivoire
- Democratic Republic of the Congo
- Djibouti
- Ethiopia
- Gaza
- Germany
- Guinea
- Israel
- Laos
- Namibia
- Niger
- Nigeria
- Pakistan
- Papua New Guinea
- Poland
- Senegal
- Somalia
- South Sudan
- Sudan
- Tanzania
- United Kingdom
- Yemen
The CDC issued a 'Level 2' advisory, which means to 'practice enhanced precautions'.
The advisory suggests that children and adults should be up to date on their routine polio vaccines. Travelers are also asked to get an inactivated polio vaccine booster if they are going to the destination that has circulating poliovirus, or have completed their routine polio vaccine series; and have not already received one adult booster dose.
Also Read: Colon Cancer Is The Leading Cause Of Death In US For People Under 50
If Polio Has Been Eliminated In The US, Then Why Do Travelers Need Advisory?
Dr Leana Wen, CNN wellness expert, who is an emergency physician and adjunct associate professor at the George Washington University said that while the US eliminated continuous transmission of polio in 1979, eradication within the country does not eliminate the risk when people travel to places where the virus is still circulating.
Speaking to CNN, Wen said that the risk for any individual traveler is usually low if they are fully vaccinated, however, from a population health perspective, it is important to take the precautionary steps. "Even a single imported case could lead to local spread in communities where vaccination coverage is low."
Types Of Notices Issued By CDC
The CDC issues four different types of notices based on the gravity of the disease spread.
Level 1 : Practice Usual Precautions
Practice usual precautions for this destination, as described in the Travel Health Notice and/or on the destination page.
Level 2: Practice Enhanced Precautions
Practice enhanced precautions for this destination. The Travel Health Notice describes additional precautions or defines a specific population at risk.
Level 3: Reconsider Nonessential Travel
Reconsider nonessential travel to this destination. The outbreak or event poses risk to travelers because limited precautions are available.
Level 4: Avoid All Travel
Avoid travel to this destination unless traveling for humanitarian aid or emergency response; there is an extreme health risk for travelers and no available precautions.
What Is Polio?
The World Health Organization (WHO) notes that it is a highly infectious disease caused by a virus that invades the nervous system and can cause total paralysis in matter of hours. The virus is transmitted by person to person spread mainly through the fecal-oral route, or less frequently, by a common vehicle, which could be either from contaminated food or water. The virus also multiplies in the intestine.
The National Institute of Health (NIH), US, notes that the virus responsible for causing Polio belongs to the Picornaviridae family.
As per the WHO, the common Polio symptoms are:
- Fever
- Fatigue
- Headache
- Vomiting
- Stiffness of the neck a
- Pain in the limbs
How Does Polio Spread?
Polio is mainly transmitted through the fecal-oral route, meaning it spreads when a person consumes food or water contaminated with the virus. It can also spread through close contact with an infected individual. The poliovirus lives in the throat and intestines of those infected, and poor sanitation, unsafe water, and inadequate hygiene greatly increase the risk of transmission, especially in communities with limited access to clean facilities.
In severe cases, polio can lead to acute flaccid paralysis, which may affect the diaphragm and throat muscles, making it difficult to breathe or swallow. Since there is no cure for polio, prevention remains the only line of defense. Raising awareness about polio vaccination is therefore essential to protect individuals, especially children, from this potentially life-threatening disease.
Middle East Crisis Disrupting Health Services, Fueling Diseases & Environmental Hazards: WHO
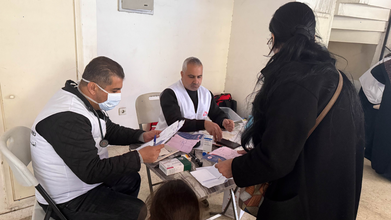
Credit: MSF/X
The ongoing conflict in the Middle East, which has stretched to more than 10 days, is disrupting health services and fueling the risk of several infectious diseases as well as environmental hazards, the World Health Organization (WHO) has said.
Citing national health authorities, the WHO reported casualties:
- Iran - over 1,300 died, 9,000 injured
- Lebanon - 570 people died and more than 1,400 injured
- Israel - 15 died and 2,142 injured.
These include:
- Iran
- 8 deaths among health workers
- Lebanon
- 16 deaths and 29 injuries to health care workers.
"The conflict is affecting the very services meant to save lives," the WHO said.
"These attacks not only cost lives but deprive communities of care when they need it most. Health workers, patients, and health facilities must always be protected under international humanitarian law,” it added.
Notably, the conflict is also collapsing health system with the shutdown of critical medical services:
- Lebanon - 49 primary health care centers and 5 hospitals shut down.
- Occupied Palestinian territory - ambulances and mobile clinics access delayed.
- Gaza - medical evacuations suspended since 28 February
- WHO’s global logistics hub in Dubai - disruption in movement of medical supplies
Francesca Quinto, Desk Manager at Doctors Without Borders, in an update social media platform X informed the threat to healthcare facilities in Lebanon.
"Our teams are witnessing the suffering up close: hospitals under pressure, communities repeatedly displaced and humanitarian needs rising sharply. Civilians and healthcare facilities must be protected and access to care and safety must be guaranteed," Quinto said.
The global health body also flagged wider public health risks due to the crisis, driving up disease risks among people displaced and living in shelter camps with limited access to safe water, sanitation, and hygiene.
As per current estimates, more than 100,000 people in Iran have relocated to other areas of the country due to insecurity, and up to 700,000 people have been internally displaced in Lebanon.
"These conditions increase the risk of respiratory infections, diarrheal diseases, and other communicable illnesses, especially for the most vulnerable populations, such as women and children," the WHO said.
Black Rain And Environmental Hazard
In addition, the Middle East crisis is also increasing concerns over environmental hazards. The petroleum fires and smoke from damaged infrastructure in Iran are potentially causing breathing problems, eye and skin irritation, and contaminated water and food sources.
Recently, Iran saw black rainfall after overnight Israeli strikes on several fuel depots caused fires to burn for hours.
Iran's Red Crescent Society had warned the residents of Tehran and the surrounding region that the rainfall after the strikes could be "highly dangerous and acidic", and could cause "chemical burns of the skin and serious damage to the lungs".
Call For De-escalation
The WHO called on all countries to de-escalate the conflict and "to protect civilians and health care, ensure unimpeded and sustained humanitarian access".
The WHO Director General, Tedros Adhanom Ghebreyesus, shared concerns about the rising global military expenditure and the rising world hunger rates.
"Global military expenditure just hit $2.7 trillion - in a single year. According to the UN estimates, ending world hunger by 2030 would require $93 billion annually. That means we spend almost 30 times more every year on killing each other than on making sure everyone eats. Numbers don't lie. Our priorities do," he said, in a post on social media platform X.
Sleep Apnea Pill Could Be The Latest Breakthrough

Credits: Canva
About 30 to 83.7 million adults in the United States have Obstructive Sleep Apnea (OSA), notes American Lung Association. Roughly 80 per cent of these cases remain undiagnosed. However, now, a simple daily pill, an old drug, could just be the solution.
Scientists in Sweden and other places too, have been studying the anti-seizure medicine sultiame as a treatment for OSA. In their latest Phase II trial, the scientists found that people on sultiame experienced an improvement in their apsea symptoms, and their sleep quality too improved as compared to those taking placebo.
The results points towards the potential of sultiame becoming an effective option for people with sleep apnea, especially those who cannot tolerate continuous positive airway pressure (CPACP) machines. The findings are published in The Lancet, and the researchers noted: "These findings offer perspective for a pharmaceutical approach to treatment of patients with obstructive sleep apnea."
Sleep Apnea Pill: What Is This Condition?
OSA is the most common form of sleep apnea, and it happens when airway muscles physically block a person's breathing during sleep. This could pause the body to wake up enough to start breathing again, only for the cycle to restart throughout the night, anywhere from five to 100 times an hour. This also causes low oxygen levels and disturb people's sleep and, over time, can raise the risk of other long-term health problems, which could include heart diseases and even dementia.
What CPAP machines do is they use air pressure to keep the airways open during sleep. While machines are an effective way, some people have trouble using them long term, which is why some companies use less cumbersome interventions, including medicines.
Read: Harish Rana Case Highlights Why Planning For A Living Will Is Important
Sleep Apnea Pill: What Was It Used For?
Sultimae or sulthiame was first launched in the 1960s by Bayger AG as an anticonvulsant - which means, it was a drug designed to treat epilepsy and prevent seizures by stabilizing nerve cell membranes and reducing abnormal, excessive electrical activity in the brain.
What the drug does is, it inhibits carbonic anhydrase, an enzyme that plays a role in regulating our breathing. Research also suggested that this could help people with sleep apnea by preventing airway collapse. The US-based Apnimed, in collaboration with the Japenese company Shionogi & Co., Ltd., have been looking to develop sultiame as a sleep apnea treatment.
How Well Has The Sleep Apnea Pill Been Tested?
The phase II of the trial involved 298 patients. Of them were untreated, moderate and people with severe sleep apnea. The people were observed for over a 15-week period, of them, half were randomized to a placebo pill to be taken right before bed, while rest were given varying doses of sultiame.
The results showed that people who took sultiame saw a noticeable decrease in apnea symptoms and also witnessed improvements in their sleep quality and daytime sleepiness. People in the highest dose group saw the most improvement, with apnea symptoms being reduced up to 47 per cent.
“It feels like a breakthrough, and we now look forward to larger and longer studies to determine whether the effect is sustained over time and whether the treatment is safe for broader patient groups,” said study researcher Jan Hedner, a senior professor of pulmonary medicine at the University of Gothenburg.
© 2024 Bennett, Coleman & Company Limited

