
Credits: Canva
Amid Rising Pollen, Britons Advised To 'Keep Windows Shut Between 10am–3pm' To Prevent Hay Fever
As birch pollen peaks throughout the UK this spring, health experts are warning of the worsening hay fever season and advising key protective measures. Spring in the UK isn't all about flowers blooming and sunshine, it's also the height of hay fever season. Health experts and the UK Met Office now implore residents across the country to take an unprecedented but crucial step- shut windows and doors between 10am and 3pm, especially in areas of high pollen. It comes after a sudden increase in tree pollen, particularly birch, which is forecast to hit "very high" levels in many areas this week.
Pollen counts in the air usually rise from mid-morning to mid-afternoon. During that window, when the sun becomes more intense and wind speeds increase, pollen becomes airborne and is more prevalent. Sealing your doors and windows during this time frame can greatly reduce your exposure.
“It’s extremely beneficial to keep windows and doors closed during certain hours of the day, particularly when it’s windy,” explained a Met Office spokesperson. “Right now, we’re in tree pollen season, with birch being the most dominant and allergenic.”
These alerts are based on ideal conditions for pollen dispersal: warm, dry weather, low rainfall, and wind. Unfortunately for allergy sufferers, that’s exactly what the UK has experienced in recent weeks.
What's Causes Hay Fever?
The culprit of this year's worst allergy onslaught? Birch pollen.
Tree pollen season typically begins in March and lasts until mid-May. Birch trees, one of the UK's most allergenic tree species, are booming this year after ideal growing conditions last spring and summer. According to the Met Office, this has led to above-average levels of pollen.
Tree pollen affects around 25% of hay fever sufferers, but this could be more this year as a result of the record amounts seen in most parts of the nation.
Hay Fever Symptoms
Hay fever, or seasonal allergic rhinitis, affects more than 10 million people in the UK. It occurs when pollen enters the body and the immune system reacts by treating it as a foreign invader, producing histamines that induce symptoms such as:
- Sneezing
- Watery, itchy eyes
- Runny or blocked nose
- Sore or itchy throat
- Sleep and tiredness
In some cases, hay fever can exacerbate asthma symptoms, leading to wheezing, coughing, and shortness of breath.
How to Protect Yourself This Season?
Although hay fever cannot be avoided, there are some good methods to minimize exposure and alleviate symptoms:
- Consult local pollen predictions and limit outdoor activity low at peak times.
- Keep doors and windows shut, especially between 10am and 3pm.
- Use home air cleaners or HEPA filters in your vehicle.
- Shower and launder after spending time outside to eliminate pollen grains.
- Use antihistamines or nasal sprays—many are available over the counter.
- Rinse pollen from nasal passages with a saline solution.
These easy actions can make a dramatic difference in quality of life in spring and summer.
Where Pollen Levels Are 'Very High' This Week
According to the latest pollen forecast map published by the Met Office, the following regions are of concern with extremely high pollen concentration:
Monday: East of England, London, South East, East Midlands
Tuesday: West Midlands, East Midlands, Eastern England, London, South East
Wednesday and Thursday: London, Kent, Sussex, Surrey, Essex, Suffolk, Norfolk, Cambridgeshire
When to Seek Doctor Help?
If symptoms persist with over-the-counter medication, or hay fever begins to disrupt activities, consult a medical doctor. Allergy testing, prescription medication, or perhaps even immunotherapy (allergy shots) might be needed for long-lasting relief.
Hay fever is usually underestimated, but in severe cases, it can impact sleep, focus, and general well-beingparticularly in children, seniors, and individuals with asthma.
Rare 100% Deadly Brain Disease Kills Two In Oregon County, Third Infection Confirmed
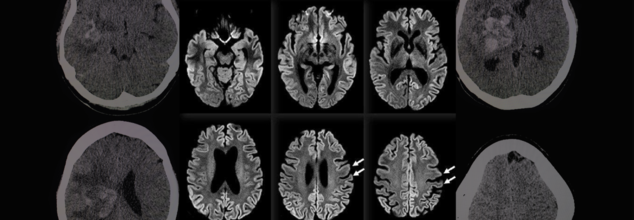
A rare and fatal brain disease with a 100% mortality rate has gripped Hood River County, Oregon, raising concerns within the medical community and eliciting intense probes by local and federal health officials. It is called Creutzfeldt-Jakob Disease (CJD), and it has killed two people and impacted a third in eight months—a terrifying cluster in a county of only slightly more than 23,000 people.
On April 14, the Hood River County Health Department reported one case of Creutzfeldt-Jakob Disease and two more probable cases. Although only one case has been confirmed by a diagnosis through an autopsy, the other two are presumptive and await post-mortem confirmation through examination of brain tissue and cerebrospinal fluid. Such examination, as explained by Trish Elliott, Director of the Hood River County Health Department, may take months.
Although the origins of these three cases are still unknown, the cluster is epidemiologically significant. The U.S. experiences about 350 cases of CJD each year, or 1 to 2 cases per million individuals globally. For Hood River County, with only 23,000 people, to see three cases over such a brief time span is an epidemiologic outlier.
What Is Creutzfeldt-Jakob Disease (CJD)?
Creutzfeldt-Jakob Disease is a rapidly advancing and always lethal neurodegenerative disease resulting from misfolded proteins known as prions. Initially documented in the 1920s by German physicians Hans Gerhard Creutzfeldt and Alfons Jakob, CJD causes sponge-like holes to form within the brain, destroying its structure and function.
CJD is a member of the larger family of prion diseases, which also encompasses other rare but fatal disorders like kuru and fatal familial insomnia. Similar to bovine spongiform encephalopathy (BSE), commonly referred to as mad cow disease, CJD irreversibly destroys the brain and has no cure.
CJD Symptoms and Progression
The symptoms of CJD are extreme and worsen quickly. Early symptoms may involve confusion, disorientation, personality changes, memory loss, visual disturbances, and stiffness of the muscles. Later in the disease, patients can develop hallucinations, difficulty speaking or swallowing, seizures, and sudden jerky movements.
Death typically occurs within a year of the onset of symptoms, usually as a result of complications such as pneumonia, heart failure, or problems arising from neurological deterioration such as falls and choking.
Symptoms in the early stages of sporadic CJD usually resemble other dementias but worsen with terrifying rapidity. The majority of individuals with sporadic CJD are between 50 and 80 years of age, but some genetic forms can occur earlier, even in some people as young as 30.
Various Types of CJD
CJD comes in several types:
Sporadic CJD (sCJD): This type is the most prevalent, affecting about 85% of the cases. This type happens spontaneously when healthy proteins in the brain misfolded into prions for unknown reasons.
Genetic CJD (fCJD): Due to mutations in the PRNP gene, this form is inherited and represents about 10–15% of the total cases. The PRNP gene codes for the prion protein (PrP), a protein involved in neuronal communication and protection.
Acquired CJD (also referred to as iatrogenic or variant CJD): This is a rare type that involves outside sources of infection, such as eating infected beef (BSE/mad cow disease) or through tainted medical equipment or transplanted tissue.
In spite of concerns, authorities from Hood River County stressed that the present cases do not seem to have resulted from infected cows. "At this point in time, there is no cause identified between these three cases," the department noted. They also pointed out that CJD cannot be transmitted via air, touching, social contact, or water.
Public Health Measures and Continued Investigations
The Hood River County Health Department, in collaboration with the Oregon Health Authority and the Centers for Disease Control and Prevention (CDC), has launched an "active and ongoing investigation" into the three reported cases.
“We’re trying to look at any common risk factors that might link these cases,” Trish Elliott told The Oregonian. “But it’s pretty hard in some cases to come up with what the real cause is.”
Although risk to the general population is "extremely low," the health department continues to monitor it. Since CJD cannot be definitely diagnosed until after death, real-time monitoring is not easy, and so robust surveillance is essential.
Can CJD Be Prevented?
Although there is no treatment or cure to prevent the development of CJD, the U.S. has established strict public health measures to minimize the risk of acquired CJD, especially through food supply control and medical safety measures.
Federal authorities have maintained since the 1990s a prohibition against feeding cattle which could be contaminated with BSE, and employment of high-risk material in foods is strictly barred. Sterilization processes of surgical devices as well as strict donor screening in transplantation and transfusions are all undertaken to cut back on iatrogenic spread.
While medical officials wait for further verification and possible connections between the three patients, the attention is on education, surveillance, and reassurance to the public.
Although it is reassuringly ominous to witness a disease of this kind emerging in a small American community, the risk at the international level remains low, especially with measures presently in place. Nevertheless, the cases are a sobering reminder of the enigma that prion diseases continue to pose to modern medicine.
Health officials are still keeping an eye on the matter and are asking people not to panic but to remain updated. "The health department will remain vigilant and inform you of any public health risk," officials promised in a statement.

Credits: Canva
Medical Cannabis May Help Fight Cancer, Largest-Ever Study Shows Potential To Treat Symptoms
The largest-ever scientific study on cannabis and cancer has shown strong evidence that medical cannabis can do more than treat symptoms — it could actually fight the disease itself. The research, published in Frontiers in Oncology, provides a robust and data-heavy analysis that brings much-needed clarity to a very contentious issue.
Led by Ryan Castle, Research Director of the Whole Health Oncology Institute, this revolutionary analysis converges more than 10,000 studies — the largest such inquiry into medical cannabis and cancer to date.
Cannabis has been in the middle of medical controversies and legislative wars for a long time. Traditionally, the Schedule I status of cannabis under federal law has limited high-quality human clinical studies, preventing the medical community from reaching a consensus. Castle and his colleagues aimed to change that.
Our aim was to establish the scientific consensus on the issue of medical cannabis, an area that has been long dominated by a war of cherrypicked studies," Castle said.
In order to transcend prejudice, Castle's team took the large-scale, inclusive approach fuelled by AI and sentiment analysis — a process widely employed by natural language processing to determine whether written material portrays a positive, neutral, or negative sentiment. Here, AI analyzed thousands of abstracts and conclusions drawn in scientific literature to determine whether each one stated agreement, neutrality, or doubt in cannabis's applicability to the treatment of cancer and symptom alleviation.
The result? An overwhelming majority of studies presented a positive view, indicating medical cannabis holds therapeutic value not just for symptom relief — such as reducing inflammation and nausea or boosting appetite — but potentially for accelerating apoptosis, the death of cancer cells.
Castle's group examined over 10 times the amount of research examined in any other meta-analysis. Their report stated that roughly 55% of studies indicated a positive relationship between medical cannabis and favorable cancer outcomes with only a few percent reporting adverse effects or none at all.
That percentage — 55% — may seem humble, but with the sheer scale of the data and the scientific conservative tradition in this area, it's telling. "This level of statistical consensus is precisely what we required to start thinking of cannabis as more than an edgy cure-all," Castle wrote.
In addition, the National Cancer Institute (NCI) revealed that 20% to 40% of patients with cancer currently use marijuana products to deal with side effects such as constant pain, chemotherapy-related nausea and vomiting, and sleeplessness. Still, investigations had fallen behind trend usage rates based on government policy and availability of funds in the past.
It is valuable to place the results of this mega-study in the context of the overall body of cannabis research. Much of what is published is derived from in vitro (test tube) experiments or animal models and not human trials. However, several of these studies have promising results: compounds found in cannabis — particularly cannabinoids such as delta-9 THC, CBD, and CBG — have been shown to inhibit cancer growth, prevent metastasis, and cause cancer cell death in laboratory experiments.
A 2023 Discover Oncology study supported this perspective, reaching the conclusion that multiple cannabinoids reveal "promising potential as anticancer agents by multiple mechanisms." These include curbing tumor expansion, inhibiting cancer cell invasion, and cutting inflammation — which is a documented driver of cancer growth.
In addition, more recent studies have discovered unforeseen advantages in cancer patients who use cannabis. A University of Colorado study reported that patients who consumed marijuana products from licensed dispensaries for a two-week period reported better thinking and cognition, contrary to previous concerns that cannabis would impair mental sharpness in chronic users.
Even with all the encouraging results, Castle and other specialists advise not to consider cannabis a panacea. The available evidence does not indicate that medical cannabis by itself can heal cancer. Rather, its actual strength is in integrative oncology — as an adjunct therapy in addition to standard therapies such as chemotherapy, radiation, and immunotherapy.
This is in agreement with results of a 2019 literature review, which noted that cannabis potentially slows cancer growth and aids improved treatment outcomes, although its effectiveness is highly variable based on cancer type, formulation of cannabinoids, and dose.
One of the significant challenges that persist in holding back development in this arena is the federal classification of cannabis as a Schedule I drug. According to existing U.S. policy, cannabis is listed alongside drugs such as heroin — a designation that presents many legal and bureaucratic hurdles to researchers and healthcare professionals.
In addition, in the Trump era, the National Cancer Institute highlighted marijuana as one of almost two dozen "controversial or high-profile issues" that needed extra clearance prior to publication or research sharing. This culture of fear and repression has only held back the much-needed research into medical cannabis's complete potential.
The biggest-ever analysis of medical cannabis and cancer isn't asserting to have discovered a cure but what they have discovered is a mounting scientific concurrence that medical cannabis should be included in mainstream discussions of cancer treatment. From reducing side effects to having the potential to interfere with cancer cell life cycles, cannabis might have more than just palliation to provide — it might have clinical benefit.

Dr. Mathew Kalarickal, 'The Father of Angioplasty' In India Passes Away At 77; How The Procedure Transformed Heart Care?
Dr. Mathew Samuel Kalarickal, a pioneer of interventional cardiology, has passed away on April 18, 2025, in Chennai, at the age of 77, marking an end to an era in coronary angioplasty and stenting technology. Popularly known as the 'Father of Angioplasty in India,' Dr. Kalarickal transformed heart care, changing the lives of thousands of patients and redefining the face of contemporary interventional cardiology.
Born on January 6, 1948, in Kerala, Dr. Kalarickal's journey to becoming one of the world's most renowned cardiologists was set early in life. After completing his medical studies at Kottayam Medical College, he went on to pursue specialization in cardiology from Chennai but his stint in the United States of America, under the guidance of Dr. Andreas Gruentzig—the man universally accepted as the 'Father of Coronary Angioplasty'—would establish the foundation for his groundbreaking career.
Dr. Kalarickal's return to India in 1985 proved to be turning point. Coronary angioplasty was a new, unexplored area in India at that time, and one that fell behind progress in the U.S. and Europe. Sensing this lacuna, Dr. Kalarickal chose to introduce this revolutionary procedure to India, with a vision of making lifesaving heart procedures reach more people.
First Angioplasty in India
In 1986, Dr. Kalarickal performed the very first angioplasty in India, a process which would subsequently alter the direction of heart treatment in the country. Angioplasty at that time was not a widely known procedure in India, and coronary artery disease was on the rise. During the first year, he had only treated 18 patients. But by 1987, that figure had risen to 150, an unmistakable indicator of both the increasing demand for this life-saving operation and the confidence that patients had in Dr. Kalarickal's skills.
His success in India did not remain confined to its borders, Dr. Kalarickal played a key role in setting up angioplasty centers in various nations in the Asia-Pacific region, such as Pakistan, Bangladesh, Sri Lanka, the United Arab Emirates, Indonesia, Thailand, and Malaysia. His relentless efforts to educate and train physicians in these nations helped ensure that this new technique spread like wildfire, eventually saving countless lives and making heart procedures more available worldwide.
Role of Dr. Kalarickal in Expanding Angioplasty Globally
Dr. Kalarickal's role was not just to bring angioplasty to India and the rest of the region. As an innovator, he was a pioneer in bringing new innovations to the world of angioplasty and stenting. One of his greatest feats was becoming the first Indian cardiologist to introduce and practice the application of drug-eluting bio-absorbable stents, which improved the efficacy of angioplasty by a large margin and minimized the threat of re-blockage in coronary arteries.
Having done more than 10,000 angioplasties, Dr. Kalarickal's expertise and commitment to improving heart health were second to none. He also contributed significantly to academia, establishing the National Angioplasty Registry of India, through which data on angioplasty operations could be gathered and analyzed to streamline and enhance practice nationwide. His contributions had an effect on the medical fraternity and made him a mentor to numerous budding cardiologists in India and overseas.
Dr. Kalarickal's success was not limited to the operating room. His leadership positions in major medical societies demonstrate his reputation as a world leader in interventional cardiology. He was president of the Asian-Pacific Society of Interventional Cardiology from 1995 to 1997 and then went on to chair the Asian-Pacific Society of Cardiology section of Interventional Cardiology between 1995 and 1999. His presidency in these societies promoted the use of angioplasty and stenting procedures around the world and consolidated the group of cardiologists in Asia.
His work was duly appreciated in many awards and honors. Dr. Kalarickal received the esteemed Padma Shri award in 2000, one of the highest civilian awards in India, for his outstanding work in cardiology. He was also awarded the Dr. B.C. Roy Award in 1996 for his notable contributions to medicine, the Doctor of Science Award by Dr. M.G.R. University in 2003, and a Lifetime Achievement Award in 2008.
While Dr. Kalarickal was well-known for his medical knowledge, he was as much admired for being a mentor. Dr. Sai Satish, who is a senior interventional cardiologist in Chennai, was trained by Dr. Kalarickal and collaborated with him for more than two decades. Talking about his experiences during his mentor's time, Dr. Satish stated, "There will never be another Dr. Mathew Samuel Kalarickal in my life.". He taught me in ways that few people ever managed, and I will miss him every time I enter a cath lab." This is a sentiment shared by many other cardiologists who were fortunate enough to learn from him. His dedication to educating and empowering the future generation of heart doctors has left an invaluable legacy on the specialty of cardiology.
Dr. Kalarickal's contributions have saved thousands of lives, and his legacy will never be lost in the profession of interventional cardiology. His vision, commitment, and pioneering attitude have revolutionized heart disease treatment in India and across the globe. With the advent of angioplasty, he revolutionized the procedure that used to be an extremely invasive and dangerous one and turned it into a routine, life-saving one.
How Angioplasty Saves Your Heart?
Angioplasty is a minimally invasive procedure to open up narrowed or blocked coronary arteries due to a buildup of fatty plaques. Plaque buildup in the arteries over time can limit blood supply to the heart, resulting in angina (chest pain) or even heart attacks. Angioplasty is done to relieve these blockages, restore normal blood flow, and prevent heart-related complications. But in what way precisely does angioplasty save the heart?
While undergoing angioplasty, a catheter is inserted into the clogged artery with a balloon at the end. The catheter is advanced through the bloodstream with great caution until it enters the area where the blockage is. Having reached its destination, the balloon is inflated, pushing the plaque against the artery walls, effectively opening up the artery and reinstating blood circulation to the heart. In most instances, a tiny mesh tube known as a stent is also inserted to keep the artery open and prevent it from closing again.
Angioplasty can be carried out in patients with different types of coronary artery disease, such as patients who have experienced heart attacks, those with chronic angina, and those at high risk for cardiac events due to plaque deposition. Angioplasty is commonly carried out on patients who are not ideal candidates for standard open-heart surgery.
Instant Relief and Long-term Advantages
Perhaps the greatest benefit of angioplasty is the relief that it brings promptly to the patient. Post-procedure, patients can notice dramatically decreased symptoms of chest pain, shortness of breath, and tiredness, all typical with clogged arteries. The normalization of blood flow tends to keep the heart from working as hard and lowers the risk of heart attacks.
In the long run, angioplasty ensures that the heart is not subjected to further harm by providing it with a sufficient supply of oxygenated blood. This is particularly vital in individuals suffering from coronary artery disease because continuous blood flow is crucial to maintaining heart muscle health. Angioplasty can greatly eliminate the risk of heart failure, heart attack, or stroke by opening up clogged arteries. Also, the procedure has been demonstrated to enhance quality of life in general, since patients are frequently able to resume normal activities following the procedure without the restrictions created by chest pain and other symptoms.
© 2024 Bennett, Coleman & Company Limited

