
5 Nurses Diagnosed With Brain Tumors On Same Floor: Is It A Cancer Cluster?
Five nurses from the same fifth-floor maternity unit at a Massachusetts Hospital have been diagnosed with brain tumors. While the tumors have been classified as benign, the unusual cluster has raised questions about potential environmental or occupational exposures within the facility. The affected nurses, all of whom worked closely on the same ward, have begun to speak out—sharing personal accounts and seeking clarity amidst growing unease. Although hospital officials report no environmental threats following internal assessments, the Massachusetts Nurses Association has launched an independent investigation, citing gaps in the original review. This unfolding situation not only brings attention to occupational health risks in clinical environments but also underscores the importance of thorough, transparent, and science-led responses to emerging health concerns in healthcare settings.
In a startling development that has raised serious concerns about occupational safety and long-term health risks within healthcare facilities. The cases, all linked to the fifth-floor maternity unit of Newton-Wellesley Hospital near Boston, have triggered an ongoing independent investigation amid claims that the hospital's initial response was insufficient.
The cluster of tumor diagnoses—part of a broader set of health concerns raised by at least 11 employees—has reignited debates around environmental exposure, transparency in institutional health investigations, and the rights of healthcare workers.
For nurses on the maternity floor at Newton-Wellesley Hospital, the news of colleagues being diagnosed with brain tumors was initially dismissed as coincidental. But when more nurses began to come forward—each with similar diagnoses—the pattern became too disturbing to ignore.
One nurse, who has asked to remain anonymous, described feeling an increasing sense of unease. “It’s getting to the point where the number just increases, and you start saying, ‘Am I crazy thinking this?’” she said. “This can’t just be a coincidence.”
According to this nurse, nearly ten nurses who have worked long-term on the fifth floor have been diagnosed with tumors over the last few years, some cancerous and some benign. At least three of these individuals have already undergone surgery. Despite these serious medical developments, she believes the hospital’s support has been inadequate. “We want reassurance, because this has not been a reassuring past few months for a lot of the staff members,” she added.
In response to the concerns, Newton-Wellesley Hospital—part of the Mass General Brigham network—initiated an internal investigation in December. A joint statement from Associate Chief Medical Officer Dr. Jonathan Sonis and Chief Nursing Officer Sandy Muse emphasized the hospital’s commitment to safety and transparency.
“We conducted an extensive investigation in collaboration with the Department of Occupational Health and Safety, radiation and pharmaceutical safety offices, and external environmental consultants,” the statement said.
Environmental assessments were conducted in accordance with CDC guidelines, including evaluations of air quality, radiation exposure, and other potential hazards on the fifth-floor unit. Hospital officials maintain that these assessments have revealed no link between the work environment and the development of brain tumors. All affected nurses were individually interviewed, and their medical histories and risk factors were taken into account.
“Based on these results, we can confidently reassure our dedicated team members and all our patients that there is no environmental risk at our facility,” the statement added.
Despite the hospital’s conclusions, the Massachusetts Nurses Association (MNA), which represents many of the affected staff members, remains unconvinced. Spokesperson Joe Markman has publicly criticized the hospital’s investigative scope and approach.
“The hospital only spoke to a small number of nurses, and their environmental testing was not comprehensive,” Markman said. “The hospital cannot make this issue go away by attempting to provide a predetermined conclusion.”
As a result, the MNA has launched its own independent investigation, working with environmental scientists and occupational health experts to evaluate whether an undiscovered factor may be at play. “Right now, the best way we can help is to complete an independent, scientific investigation. That effort is underway and may take additional weeks,” Markman noted.
What are Meningiomas?
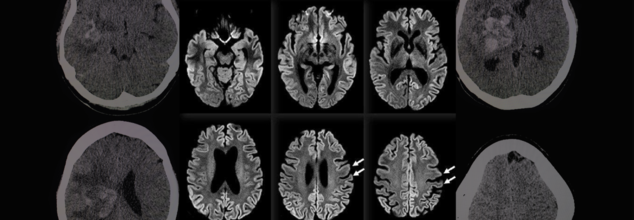
Of the five confirmed brain tumor cases, at least two nurses were diagnosed with meningiomas—the most common type of benign brain tumor in adults. While non-cancerous, these tumors can still cause significant neurological complications and require surgical removal.
According to the American Brain Tumor Association, meningiomas account for approximately 30% of all primary brain tumors. Though often slow-growing, their cause remains largely unknown. Some environmental and occupational factors have been hypothesized, including prolonged exposure to radiation or certain industrial chemicals, but definitive links are rare and difficult to prove.
The appearance of multiple cases within a confined geographic or occupational setting, however, is unusual enough to merit deeper investigation.
While Newton-Wellesley Hospital has stood by its findings, the incident has sparked broader conversations in healthcare circles. Nurses, often the backbone of any hospital, are regularly exposed to stressful environments, long working hours, and, in some cases, hazardous substances.
Workplace illness clusters have historically led to crucial discoveries about environmental exposure—think asbestos in shipyards or radiation in early radiology labs. Whether this situation at Newton-Wellesley turns out to be another such case remains to be seen.
What Are Cancer Clusters?
A cancer cluster refers to an unusually high number of cancer cases—typically the same type—occurring within a defined group of people, geographic location, or occupational setting over a particular period. These clusters often surface through anecdotal observation, with individuals or communities raising concerns after noticing an unexpected concentration of cancer diagnoses among colleagues, neighbors, or family members.
Notably, cancer is unfortunately common—particularly in aging populations. For example, in places like Queensland, Australia, data shows that one in two men and one in three women are likely to develop cancer by the age of 80. Because of this high baseline incidence, it is not uncommon for several cases to appear in one community or workplace simply by chance, without any shared cause or exposure.
Still, certain patterns merit deeper investigation. A suspected cancer cluster is more likely to be considered a confirmed cancer cluster when:
- All or most cases are of the same type of cancer
- The cancer type is rare or unusual for the population group
- It affects people in uncharacteristic age groups
There is known exposure to a carcinogenic agent, such as radiation, chemicals, or environmental toxins
Even then, confirmation is rare. Historically, most suspected cancer clusters do not show statistical significance, with only 5–15% found to be meaningfully above expected rates upon epidemiological analysis. The rest are often attributable to random distribution, as even in large, well-studied populations, uneven geographic or social clustering of cases can occur purely by chance.

Credits: Canva
World Liver Day: How A Timely Liver Transplant Saved A 30-Year-Old Man
On World Liver Day, which is observed on April 19, to spread awareness about liver health and the life-saving power of organ donation, let us look at one such real-life story. This is where doctor's prompt's action and one's selfless donation saved one human's life.
When the 30-year-old Delhi-based man walked into the hospital, he had yellow eyes and dangerously high liver enzymes. He was admitted in Max Super Speciality Hospital, Patparganj. That moment, he rarely knew that his life was, in fact, hanging by a thread. The man was diagnosed with acute liver failure, which was caused by viral hepatitis. His body was slowly shutting down. The frequency of his body shutting down had increased. The doctors also quickly informed the family. This was the one last hope of survival - a liver transplant.
The First Option Failed
His sister was family's first ray of hope. She was also willing and had a compatible liver whose part of it could be donated. However, pre-surgery tests revealed that her liver size was too small to ensure a safe transplant. The family then proposed the patient's brother-in-law - a second-degree relative, as the next donor. His liver was a better match, but since he was not an immediate blood relative, there had to be special regulatory approvals which were required.
However, the worsening condition of the patients allowed no such time.
The hospital too scrambled to get clearance for the brother-in-law. All this while, the patient suffered a cardiac arrest. The situation turned dire within minutes. Doctors performed CPR to revive him. He was immediately put on ventilator support. The decision had to be taken soon.
A Miraculous Surgery
With no time in hand, the doctors decided to go ahead with the sister as the donor, though there were risks there too.
A team of highly skilled hepatobiliary surgeons, anesthesiologists, and critical care specialists took over. In a high-risk, nine-hour surgery, they removed the patient’s failing liver and replaced it with part of his sister’s.
“This was one of the most challenging cases we’ve handled,” said Dr. Ajitabh Srivastava, Director – HPB Surgery & Liver Transplant. “When the patient collapsed, our team acted within seconds. Every decision, every move mattered. His survival was truly a team triumph.”
The patient is now recovering well.
What Is A Liver Transplant?
As per the National Institute of Diabetes and Digestive and Kidney Diseases, a liver transplant is a surgical procedure to replace a diseased liver with a healthy one from a donor. It’s often the last resort when liver failure occurs—whether due to chronic illness or sudden injury.
When Is It Needed?
People may need a liver transplant for:
- Alcoholic liver disease
- Fatty liver disease (NASH)
- Cirrhosis due to chronic hepatitis C
- Liver cancer with cirrhosis
- Acute liver failure (often due to drug overdose, hepatitis, or toxins)
Types of Liver Transplants
Deceased Donor Transplant:
The most common type, where a full or partial liver is taken from someone who has recently died.
Living Donor Transplant:
A healthy person donates a portion of their liver—typically a close relative. Both the donor’s and recipient’s liver regenerate to normal size in a few weeks.
What Must Be Kept In The Mind?
- Matching and Compatibility: Blood type, liver size, and health are crucial.
- Approval Process: Especially important for non-blood relatives.
- Recovery and Monitoring: Post-op care involves lifelong medication, lifestyle changes, and regular check-ups.
Rare 100% Deadly Brain Disease Kills Two In Oregon County, Third Infection Confirmed
A rare and fatal brain disease with a 100% mortality rate has gripped Hood River County, Oregon, raising concerns within the medical community and eliciting intense probes by local and federal health officials. It is called Creutzfeldt-Jakob Disease (CJD), and it has killed two people and impacted a third in eight months—a terrifying cluster in a county of only slightly more than 23,000 people.
On April 14, the Hood River County Health Department reported one case of Creutzfeldt-Jakob Disease and two more probable cases. Although only one case has been confirmed by a diagnosis through an autopsy, the other two are presumptive and await post-mortem confirmation through examination of brain tissue and cerebrospinal fluid. Such examination, as explained by Trish Elliott, Director of the Hood River County Health Department, may take months.
Although the origins of these three cases are still unknown, the cluster is epidemiologically significant. The U.S. experiences about 350 cases of CJD each year, or 1 to 2 cases per million individuals globally. For Hood River County, with only 23,000 people, to see three cases over such a brief time span is an epidemiologic outlier.
What Is Creutzfeldt-Jakob Disease (CJD)?
Creutzfeldt-Jakob Disease is a rapidly advancing and always lethal neurodegenerative disease resulting from misfolded proteins known as prions. Initially documented in the 1920s by German physicians Hans Gerhard Creutzfeldt and Alfons Jakob, CJD causes sponge-like holes to form within the brain, destroying its structure and function.
CJD is a member of the larger family of prion diseases, which also encompasses other rare but fatal disorders like kuru and fatal familial insomnia. Similar to bovine spongiform encephalopathy (BSE), commonly referred to as mad cow disease, CJD irreversibly destroys the brain and has no cure.
CJD Symptoms and Progression
The symptoms of CJD are extreme and worsen quickly. Early symptoms may involve confusion, disorientation, personality changes, memory loss, visual disturbances, and stiffness of the muscles. Later in the disease, patients can develop hallucinations, difficulty speaking or swallowing, seizures, and sudden jerky movements.
Death typically occurs within a year of the onset of symptoms, usually as a result of complications such as pneumonia, heart failure, or problems arising from neurological deterioration such as falls and choking.
Symptoms in the early stages of sporadic CJD usually resemble other dementias but worsen with terrifying rapidity. The majority of individuals with sporadic CJD are between 50 and 80 years of age, but some genetic forms can occur earlier, even in some people as young as 30.
Various Types of CJD
CJD comes in several types:
Sporadic CJD (sCJD): This type is the most prevalent, affecting about 85% of the cases. This type happens spontaneously when healthy proteins in the brain misfolded into prions for unknown reasons.
Genetic CJD (fCJD): Due to mutations in the PRNP gene, this form is inherited and represents about 10–15% of the total cases. The PRNP gene codes for the prion protein (PrP), a protein involved in neuronal communication and protection.
Acquired CJD (also referred to as iatrogenic or variant CJD): This is a rare type that involves outside sources of infection, such as eating infected beef (BSE/mad cow disease) or through tainted medical equipment or transplanted tissue.
In spite of concerns, authorities from Hood River County stressed that the present cases do not seem to have resulted from infected cows. "At this point in time, there is no cause identified between these three cases," the department noted. They also pointed out that CJD cannot be transmitted via air, touching, social contact, or water.
Public Health Measures and Continued Investigations
The Hood River County Health Department, in collaboration with the Oregon Health Authority and the Centers for Disease Control and Prevention (CDC), has launched an "active and ongoing investigation" into the three reported cases.
“We’re trying to look at any common risk factors that might link these cases,” Trish Elliott told The Oregonian. “But it’s pretty hard in some cases to come up with what the real cause is.”
Although risk to the general population is "extremely low," the health department continues to monitor it. Since CJD cannot be definitely diagnosed until after death, real-time monitoring is not easy, and so robust surveillance is essential.
Can CJD Be Prevented?
Although there is no treatment or cure to prevent the development of CJD, the U.S. has established strict public health measures to minimize the risk of acquired CJD, especially through food supply control and medical safety measures.
Federal authorities have maintained since the 1990s a prohibition against feeding cattle which could be contaminated with BSE, and employment of high-risk material in foods is strictly barred. Sterilization processes of surgical devices as well as strict donor screening in transplantation and transfusions are all undertaken to cut back on iatrogenic spread.
While medical officials wait for further verification and possible connections between the three patients, the attention is on education, surveillance, and reassurance to the public.
Although it is reassuringly ominous to witness a disease of this kind emerging in a small American community, the risk at the international level remains low, especially with measures presently in place. Nevertheless, the cases are a sobering reminder of the enigma that prion diseases continue to pose to modern medicine.
Health officials are still keeping an eye on the matter and are asking people not to panic but to remain updated. "The health department will remain vigilant and inform you of any public health risk," officials promised in a statement.

Credits: Canva
Medical Cannabis May Help Fight Cancer, Largest-Ever Study Shows Potential To Treat Symptoms
The largest-ever scientific study on cannabis and cancer has shown strong evidence that medical cannabis can do more than treat symptoms — it could actually fight the disease itself. The research, published in Frontiers in Oncology, provides a robust and data-heavy analysis that brings much-needed clarity to a very contentious issue.
Led by Ryan Castle, Research Director of the Whole Health Oncology Institute, this revolutionary analysis converges more than 10,000 studies — the largest such inquiry into medical cannabis and cancer to date.
Cannabis has been in the middle of medical controversies and legislative wars for a long time. Traditionally, the Schedule I status of cannabis under federal law has limited high-quality human clinical studies, preventing the medical community from reaching a consensus. Castle and his colleagues aimed to change that.
Our aim was to establish the scientific consensus on the issue of medical cannabis, an area that has been long dominated by a war of cherrypicked studies," Castle said.
In order to transcend prejudice, Castle's team took the large-scale, inclusive approach fuelled by AI and sentiment analysis — a process widely employed by natural language processing to determine whether written material portrays a positive, neutral, or negative sentiment. Here, AI analyzed thousands of abstracts and conclusions drawn in scientific literature to determine whether each one stated agreement, neutrality, or doubt in cannabis's applicability to the treatment of cancer and symptom alleviation.
The result? An overwhelming majority of studies presented a positive view, indicating medical cannabis holds therapeutic value not just for symptom relief — such as reducing inflammation and nausea or boosting appetite — but potentially for accelerating apoptosis, the death of cancer cells.
Castle's group examined over 10 times the amount of research examined in any other meta-analysis. Their report stated that roughly 55% of studies indicated a positive relationship between medical cannabis and favorable cancer outcomes with only a few percent reporting adverse effects or none at all.
That percentage — 55% — may seem humble, but with the sheer scale of the data and the scientific conservative tradition in this area, it's telling. "This level of statistical consensus is precisely what we required to start thinking of cannabis as more than an edgy cure-all," Castle wrote.
In addition, the National Cancer Institute (NCI) revealed that 20% to 40% of patients with cancer currently use marijuana products to deal with side effects such as constant pain, chemotherapy-related nausea and vomiting, and sleeplessness. Still, investigations had fallen behind trend usage rates based on government policy and availability of funds in the past.
It is valuable to place the results of this mega-study in the context of the overall body of cannabis research. Much of what is published is derived from in vitro (test tube) experiments or animal models and not human trials. However, several of these studies have promising results: compounds found in cannabis — particularly cannabinoids such as delta-9 THC, CBD, and CBG — have been shown to inhibit cancer growth, prevent metastasis, and cause cancer cell death in laboratory experiments.
A 2023 Discover Oncology study supported this perspective, reaching the conclusion that multiple cannabinoids reveal "promising potential as anticancer agents by multiple mechanisms." These include curbing tumor expansion, inhibiting cancer cell invasion, and cutting inflammation — which is a documented driver of cancer growth.
In addition, more recent studies have discovered unforeseen advantages in cancer patients who use cannabis. A University of Colorado study reported that patients who consumed marijuana products from licensed dispensaries for a two-week period reported better thinking and cognition, contrary to previous concerns that cannabis would impair mental sharpness in chronic users.
Even with all the encouraging results, Castle and other specialists advise not to consider cannabis a panacea. The available evidence does not indicate that medical cannabis by itself can heal cancer. Rather, its actual strength is in integrative oncology — as an adjunct therapy in addition to standard therapies such as chemotherapy, radiation, and immunotherapy.
This is in agreement with results of a 2019 literature review, which noted that cannabis potentially slows cancer growth and aids improved treatment outcomes, although its effectiveness is highly variable based on cancer type, formulation of cannabinoids, and dose.
One of the significant challenges that persist in holding back development in this arena is the federal classification of cannabis as a Schedule I drug. According to existing U.S. policy, cannabis is listed alongside drugs such as heroin — a designation that presents many legal and bureaucratic hurdles to researchers and healthcare professionals.
In addition, in the Trump era, the National Cancer Institute highlighted marijuana as one of almost two dozen "controversial or high-profile issues" that needed extra clearance prior to publication or research sharing. This culture of fear and repression has only held back the much-needed research into medical cannabis's complete potential.
The biggest-ever analysis of medical cannabis and cancer isn't asserting to have discovered a cure but what they have discovered is a mounting scientific concurrence that medical cannabis should be included in mainstream discussions of cancer treatment. From reducing side effects to having the potential to interfere with cancer cell life cycles, cannabis might have more than just palliation to provide — it might have clinical benefit.
© 2024 Bennett, Coleman & Company Limited

